Research Updates
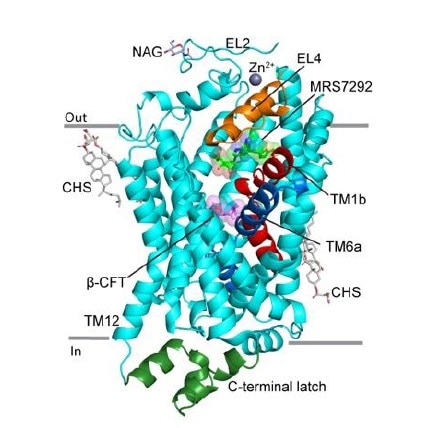
Researchers reveal the first mapped 3D structure of the human dopamine transporter
A research team including scientists from Oregon Health & Science University and the NIDDK Intramural Research Program successfully created the first high-resolution 3D structure of the human dopamine transporter (hDAT), which is targeted by anti-depressants and illicit substances to alter the uptake of the mood- and motivation-regulating molecule dopamine. The researchers used the cocaine analog β-CFT, the inhibitor nucleoside MRS7292 (developed in Ken Jacobson’s lab, NIDDK), and a zinc ion to study how hDAT’s structure changes when bound by different molecules and to understand why certain molecules prefer hDAT over other similar neurotransmitters, such as the human norepinephrine transporter (hNET) and human serotonin transporter (hSERT).
They observed β-CFT holds hDAT in an open conformation, allowing for additional dopamine release, and MRS7292 attaches to hDAT at a newly discovered site, acting as a wedge to prevent any already bound molecules from detaching. Using the mapped hDAT structure, researchers discovered the Zn2+ ion inhibits dopamine transporter activity by stitching together sites on the transporter where the molecule would normally bind.
This study, which was published in Nature in August and supported by the National Institute of Mental Health and the National Institute of General Medical Sciences, provides insight into how small molecules and ions modulate hDAT’s ability to transport dopamine.
 Credit: Nature
Credit: Nature
Opioid prescriptions decline for people on long-term dialysis or with kidney transplants
NIDDK researchers analyzing data from the United States Renal Data System found that opioid prescription rates among people in the U.S. treated with dialysis or who had a kidney transplant dropped steadily from 2011-2020. Rates fell from 60% to 42%, and 23% to 13%, respectively, with hydrocodone being the most commonly prescribed.
In the previous decade, the use of opioids in the U.S. increased markedly, including among people with end-stage renal disease (ESRD) who commonly experience pain. Between 2006 and 2010, 60% of people treated with dialysis received at least one opioid prescription each year; about 20% got chronic prescriptions. In 2010, 15% of kidney transplant recipients received chronic opioid prescriptions. The CDC issued revised opioid prescription guidelines in 2016 and 2022, suggesting the effectiveness of U.S. health care policy initiatives.
The findings, published in the Journal of American Society of Nephrology, indicate that regardless of the prescription rates within this population, short-term and chronic opioid prescriptions were associated with increased mortality and morbidity, and higher prescribed opioid doses were consistently associated with increases in deaths.
Depleting some stem cells rejuvenates the immune system
NIDDK-supported research found that depleting specific hematopoietic stem cells (HSCs) revitalized the immune systems of aged mice. Immune systems lose their ability to respond to novel infections with age, due in part to age-related changes within the HSCs themselves. Young HSCs produce a balance of lymphoid and myeloid-based cells (my-HSCs), but, over time, the number of my-HSCs increases and fewer lymphoid cells are made. This causes inflammation and a reduced ability to fight infection.
Researchers at Stanford University tested the hypothesis by depleting my-HSCs in aged mice and saw lymphoid cell production increase. More naïve T cells and B cells were present than in the blood of untreated mice. The aged mice with depleted my-HSCs also had stronger T cell responses and protection against infection. Researchers noted that the genes characterizing my-HSCs in mice were also found in aged human HSCs.
The findings, published in Nature and highlighted in NIH Research Matters, could explain why older people are more vulnerable to infections and suggest that my-HSC depletion might be used to relieve certain age-associated health problems in humans.
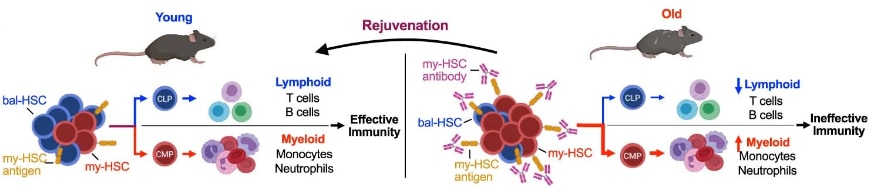
Accessible Image Description
A schematic illustration of how to rejuvenate aged immune systems in a mouse model by selective antibody-guided depletion of myeloid-biased hematopoietic stem cells, which are present at high levels versus lymphoid cells in older mice. Removal of the myeloid-biased stem cells restores a balance between lymphoid (T cells, B cells) and myeloid (monocytes, neutrophils) immune cell types in the organism, allowing them to mount effective immune responses against viral infections.
MYCT1 gene controls environmental sensing in human blood stem cells
An NIDDK-supported study identified the gene MYCT1 as playing a key role in promoting the self-renewal and growth of human haematopoietic stem cells (HSC), or blood stem cells. The researchers found that MYCT1 controls how HSCs sense and respond to environmental signals by moderating endocytosis, the process by which cells transport substances into the cell from the external environment to help them grow and develop.
MYCT1 loss led to excessive endocytosis and hyperactive signaling, undercutting HSC expression. Restoring MYCT1 balanced endocytosis and moderated signaling, suggesting MYCT1-moderated endocytosis and environmental sensing were vital for preserving human HSC stemness characteristics, such as ETS factor expression and low mitochondrial activity. A depletion of MYCT1 also prevented expansion and engraftment of human fetal liver and cord blood haematopoietic stem progenitor cells, while restoration improved them.
Published in June in Nature, the research provides insight into the self-renewal and engraftment processes of human HSCs and existing challenges of preserving and cultivating functional HSCs in culture.
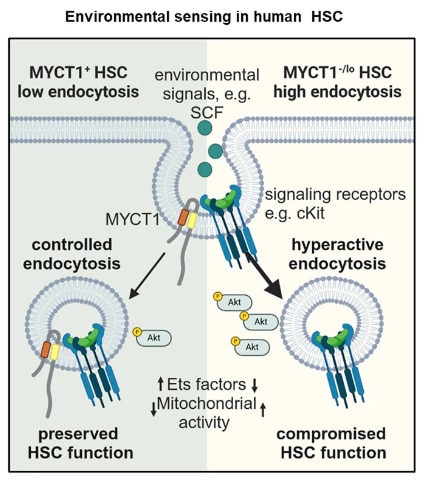
Accessible Image Description
Schematic illustration of how MYCT1 regulates human haematopoietic stem cell (HSC) function. When embedded in the HSC membrane, MYCT1 controls how a cell responds to changes in its microenvironment. A cell with MYCT1 does not ingest particles from its environment at a high-rate via endocytosis and retains its stem cell qualities, which are desirable for research. Meanwhile, a cell without MYCT1 performs endocytosis at a higher rate and begins to lose stem cell traits as it adapts to the environmental changes it can detect. Knowing MYCT1 can prevent stem cells from changing will help researchers overcome a major challenge in HSC-based research.
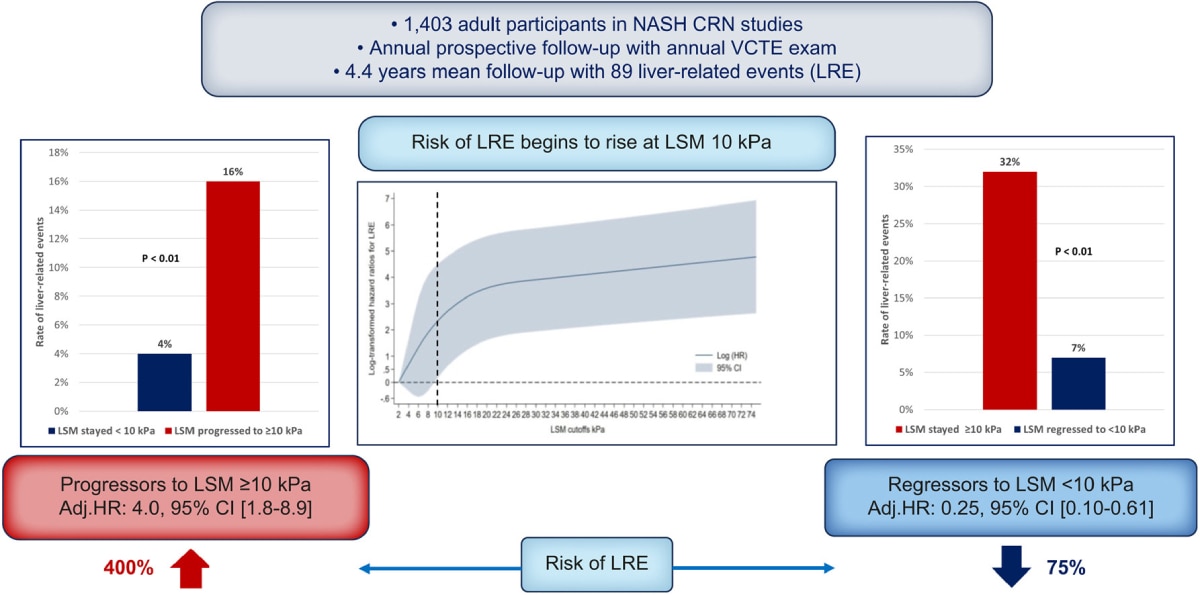
Increases and decreases in liver stiffness measurement are independently associated with the risk of liver-related events in NAFLD
NIDDK-supported research demonstrated liver stiffness measurements (LSM) can offer a non-invasive way to predict clinical outcomes in people with non-alcoholic fatty liver disease (NAFLD) over time, potentially reducing a need for serial liver biopsies.
Over 4.4 years, researchers measured liver stiffness (which indicates the presence of scar tissue) in 1,403 participants with NAFLD, tracking progression to compensated advanced chronic liver disease; sometimes referred to as advanced fibrosis or cirrhosis. Progression to higher (≥10kPa) liver stiffness measurements was independently associated with a 4x increased risk of experiencing a liver-related event, such as hepatocellular carcinoma, and regression to lower LSM (<10 kPA) was associated with a 75% decrease in risk.
The study was performed by the NIDDK Nonalcoholic Steatohepatitis Clinical Research Network (NASH CRN) and published in the Journal of Hepatology in May.
 View full-sized image
View full-sized image
Accessible Image Description
A schematic of findings gathered from an NAFLD study on liver stiffness measurements and their potential clinical applications. 1,403 adult participants in NASH Clinical Research Network (CRN) studies had an annual follow-up and vibration-controlled transient elastography (VCTE) (liver stiffness) measurement taken for 4.4 years on average. In the group, 89 liver-related events (LREs) were recorded. To illustrate their findings, three graphs are provided.
In the first bar graph, two bars are shown plotted on the x-axis – one is labelled “liver stiffness measurement (LSM) stayed <10 kPa” and the other is labelled “LSM progressed ≥10 kPa.” The y-axis is labelled “rate of liver-related events” in percentage. A 4% rate of liver-related events was observed in individuals with an LSM that stayed <10 kPa. A 16% rate of liver-related events was observed in people whose LSM progressed ≥10 kPa. Individuals with a LSM ≥10 kPa were 400% more likely to experience a liver-related event in comparison to people whose LSM remained
In the second bar graph, the x-axis is labelled “LSM cutoffs kPa” and y-axis is labelled “log-transformed hazard ratio for LRE.” It notes risk of LRE begins to rise at a LSM of 10 kPa. In the third graph, two bar graphs are shown. One is labelled “LSM stayed ≥10 kPa” and the other is labelled “LSM regressed to <10 kPa.” 32% of individuals with a LSM that stayed ≥10 kPa over the course of their follow-ups was 32% more likely to experience a liver-related event in comparison to 7% of individuals whose LSM regressed to <10 kPa. If an individual’s LSM regressed to <10 kPa, they were 75% less likely to experience a liver-related event.
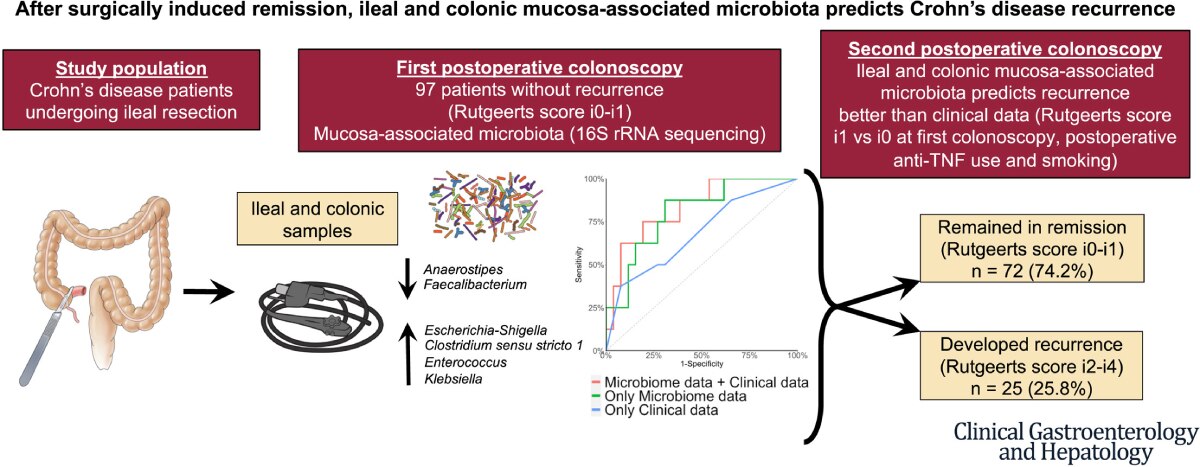
Microbiome differences predict Crohn’s disease recurrence after surgery
New research from the NIDDK-supported Inflammatory Bowel Disease (IBD) Genetics Consortium found distinctly different gut microbiomes in people who had a recurrence of Crohn’s disease after surgically-induced remission, compared to those who did not have a recurrence.
A total of 349 postoperative colonoscopies and 944 biopsy samples from 262 patients with Crohn’s disease were analyzed. Samples obtained from 97 patients who were in surgical remission at first postoperative colonoscopy and went on to develop endoscopic recurrence at second colonoscopy showed microbiome changes and lower microbial diversity, when compared with patients who remained in endoscopic remission.
The gut microbiome predicted future recurrence better than clinical features alone, suggesting that targeting the gut microbiome is a plausible approach to prevent postoperative Crohn’s disease recurrence. The research was published in Clinical Gastroenterology and Hepatology in July.
 View full-sized image
View full-sized image
Accessible Image Description
A schematic illustration depicting how, after surgically induced remission, ileal and colonic mucosa-associated microbiota can predict the recurrence of Crohn’s disease in patients.
Deriving ileal and colonic samples from Crohn’s disease patients who were undergoing ileal resection, researchers noted individuals with a depletion of genus Anaerostipes and Faecalibacterium microbiota and an increase of microbes from several genera of class Gammaproteobacteria (Escherichia-Shigella, Clostridium sensu stricto 1, Enterococcus, and Klebsiella) were at increased risk of further Crohn’s disease recurrence.
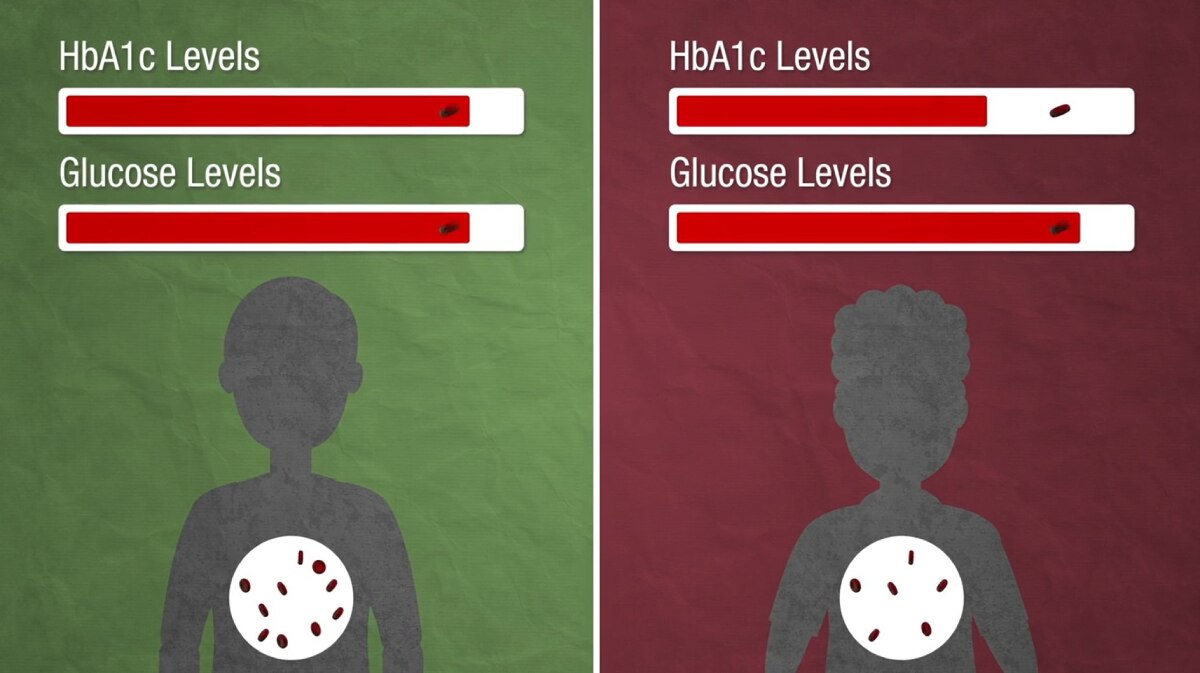
Gene variant increases risk of diabetic complications in individuals of African ancestry
A genetic variant more common in some people with African ancestry is associated with a higher risk of diabetes complications such as eye disease, according to NIH-supported research led by Vanderbilt University Medical Center and the NIH National Institute of Environmental Health Sciences. The genetic variant, glucose-6-phosphate dehydrogenase deficiency (G6PDdef) causes a more rapid turnover of red blood cells and is linked to lower levels of HbA1c, a widely used measure of blood glucose (sugar) levels that can be used to diagnose and monitor diabetes.
Despite having low HbA1c, people with G6PDdef could still be experiencing high blood sugar or have diabetes, causing a delayed diagnosis or inadequate treatment leading to an increased risk of complications. This finding suggests that HbA1c is an unreliable indicator of high blood glucose in the nearly 500 million people worldwide who have a G6PDdef variant.
The researchers estimated that about 12% of diabetic retinopathy and 9% of diabetic neuropathy cases in the United States could be prevented if diabetes screening tools for people with African descent and diabetes treatment for people with the G6PDdef variant are aimed at glucose rather than HbA1c. The findings published in Nature Medicine in June. Learn more about these findings in this video.
 Credit: Kindea Labs
Credit: Kindea Labs
Accessible Image Description
A still from a video discussing the findings of a G6PD deficiency study that depicts an individual without a G6PD deficiency (left) and one with a G6PD deficiency (right). In individuals with a G6PD deficiency, researchers found red blood cells did not last as long, causing HbA1c levels (a measurement of blood glucose) to decrease and underestimate actual glucose levels in patients with the deficiency. Because of this, individuals with a G6PD deficiency experience an increased risk of diabetes-related health consequences such as retinopathy, neuropathy, nephropathy, and cardiomyopathy.
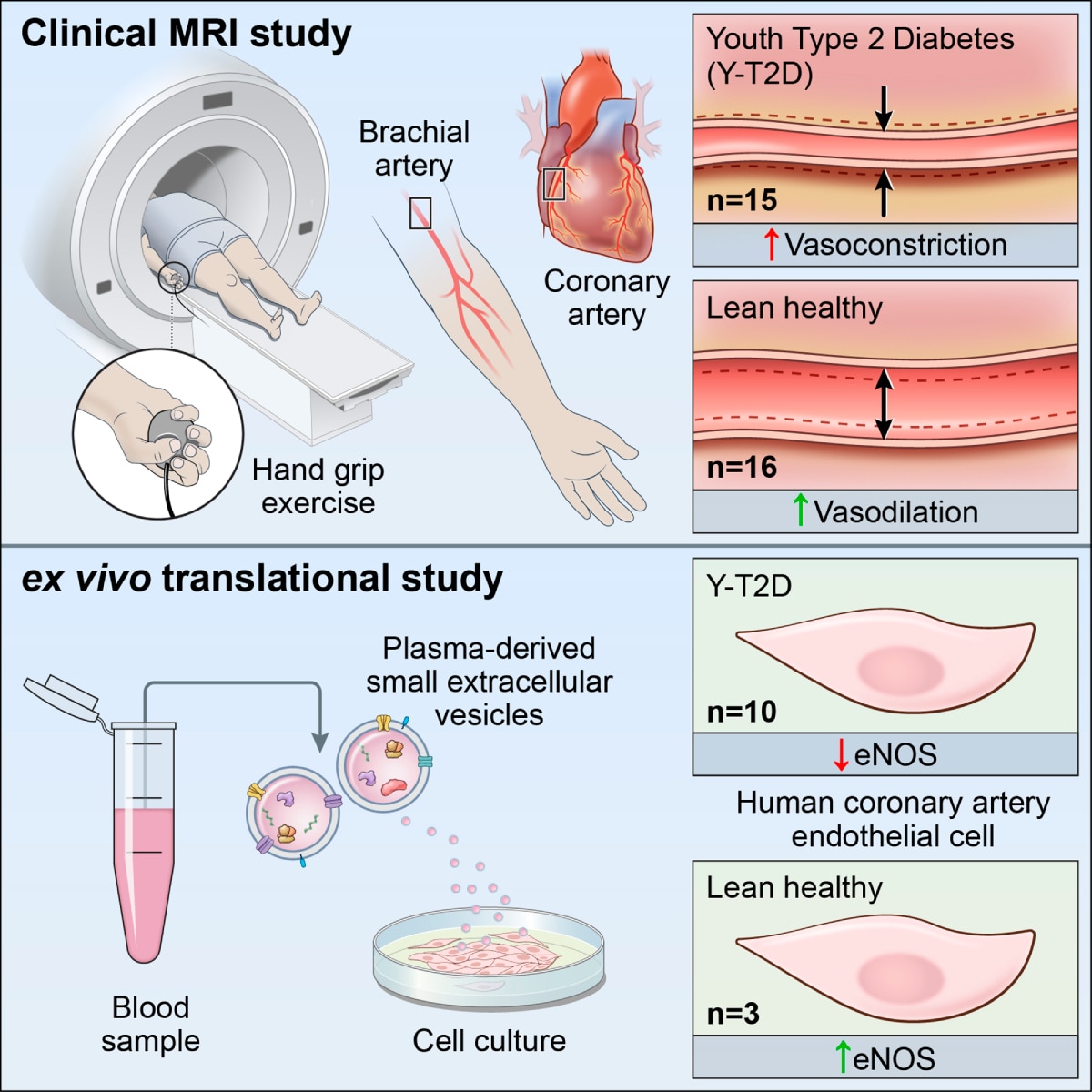
Early signs of coronary atherosclerotic disease are detectable in young people diagnosed with youth-onset type 2 diabetes
An NIDDK study has shown early-stage coronary atherosclerotic disease can be detected via novel functional MRI imaging exams and blood tests in people diagnosed with youth-onset type-2 diabetes (Y-T2D) for less than 5 years. MRIs, a non-invasive means of checking blood vessel size and function, and blood samples were gathered from 20 people over the age of 18 diagnosed with Y-T2D within the last five years and 16 healthy young people after an overnight fast. The results showed structural, functional, and biomarker-based signs of impaired blood vessel function in the coronary and brachial arteries (vessels that supply blood to the heart and arm) in young people with Y-T2D, confirming endothelial dysfunction, the earliest feature of coronary atherosclerotic disease.
The findings underscore the importance of early treatment and efforts to prevent the development and progression of heart disease in people with Y-T2D. This research was published in Circulation Research in August.
 View full-sized image
View full-sized image
Accessible Image Description
A schematic depicting the clinical magnetic resonance imaging (MRI) and ex vivo translational studies conducted to study youth-onset type 2 diabetes. In the clinical MRI study, a patient performs a hand grip exercise with their right hand, which allows the researchers to measure expansion and contraction of the right brachial artery, the major vessel that supplies blood to the upper arm, and right coronary artery, the major vessel that supplies blood to the heart. People with youth-onset T2D had thicker right coronary arteries and abnormal constriction of blood flow to the heart and arm compared to people without youth-onset T2D.
In the ex vivo translational study, researchers conducted laboratory experiments on blood samples drawn from individuals with and without youth-onset T2D. Samples from people with youth-onset T2D contained small extracellular vesicles (molecules cells use to communicate with each other) with increased inflammatory biomarkers.
New tool reveals hidden potential of existing cancer therapies
NIDDK and Purdue University researchers discovered a previously overlooked drug for bladder cancer using a new, collaboratively developed tool, the Pathway Ensemble Tool (PET), that combines multiple computational methods to identify disease-relevant biological pathways. In comparison to existing tools, which are prone to researcher bias, PET can provide novel insights by identifying unexplored treatments and biomarkers to guide clinical care. Researchers used PET to analyze 12 different types of cancers and found pathways specific to each one. Notably, PET predicted the CDK9-inhibitor CCT068127 would be an effective bladder cancer drug, a finding not implicated in existing bladder cancer research. The drug successfully halted cancer cell growth, outperforming current treatment options in animal and lab tests.
Published in Nature Communications in August, this study shows how PET and other exploratory tools may further our understanding of cancer disease mechanisms to advance treatment development. PET and other tools developed as a part of the study are available online for public use.
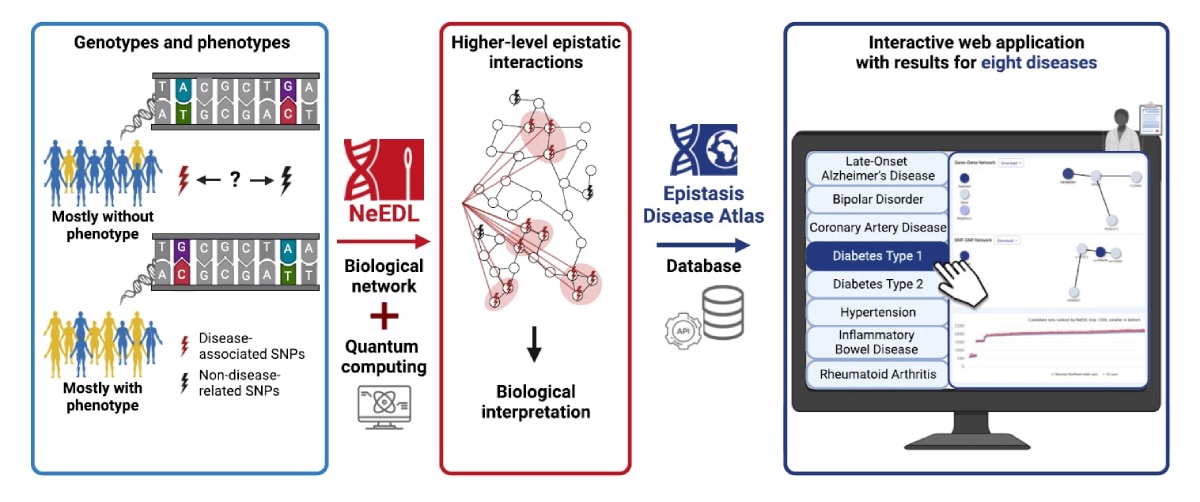
Quantum computing tool uncovers potentially relevant mutations between gene interactions in complex diseases
A team of international scientists including NIDDK researchers created a quantum computing tool, NeEDL (network-based epistasis detection via local search), to identify clinically relevant mutations between gene interactions that can influence severity and prognosis of heritable diseases, such as diabetes.
For eight diseases, NeEDL surveyed epistatic interactions, the interactions between genes that together influence a trait such as disease severity, between single nucleotide polymorphisms (SNPs), a single variation present in an individual’s genetic code. SNPs were mapped to interactions between genes, and interactions with the highest statistical significance were identified. NeEDL was applied to independent cohorts for Alzheimer’s disease and was able to replicate previously identified SNP sets, demonstrating an ability to acquire consistent results. Evaluating epistatic candidates for late-onset Alzheimer’s disease, type 1 diabetes, and inflammatory bowel disease, researchers found NeEDL mirrored existing literature and identified additional candidates that could be used to refine diagnostic criteria.
Data generated by NeEDL is accessible to the public via the Epistasis Disease Atlas, an interactive web application, for further analysis. Superseding limitations present in other epistasis detection tools, NeEDL demonstrates the potential to accelerate biomedical research with quantum computing. The study was published in Nucleic Acids Research in August.
 Credit: Nucleic Acids ResearchView full-sized image
Credit: Nucleic Acids ResearchView full-sized image
Accessible Image Description
A schematic illustration of how NeEDL uses quantum computing and biological network data to give researchers a higher-level understanding of epistatic interactions contributing to specific heritable diseases. Data generated by NeEDL is stored on the Epistasis Disease Atlas, an interactive web application, for researcher use.

