Definition & Facts for Gastritis & Gastropathy
In this section:
- What are gastritis and gastropathy?
- Are there different types of gastritis and gastropathy?
- How common are gastritis and gastropathy?
- Who is more likely to have gastritis or gastropathy?
- What are the complications of gastritis and gastropathy?
What are gastritis and gastropathy?
Gastritis and gastropathy are conditions that affect the stomach lining, also known as the mucosa. In gastritis, the stomach lining is inflamed. In gastropathy, the stomach lining is damaged, but little or no inflammation is present.
Are there different types of gastritis and gastropathy?
Experts have identified many types of gastritis and gastropathy, which have different causes.
Gastritis and gastropathy may be chronic, developing slowly and lasting a long time, or acute, developing suddenly and lasting a short time. Some forms are erosive, meaning that they wear away the stomach lining and cause shallow breaks, called erosions, and ulcers. Other forms are nonerosive.
Common types of gastritis and gastropathy include the following.
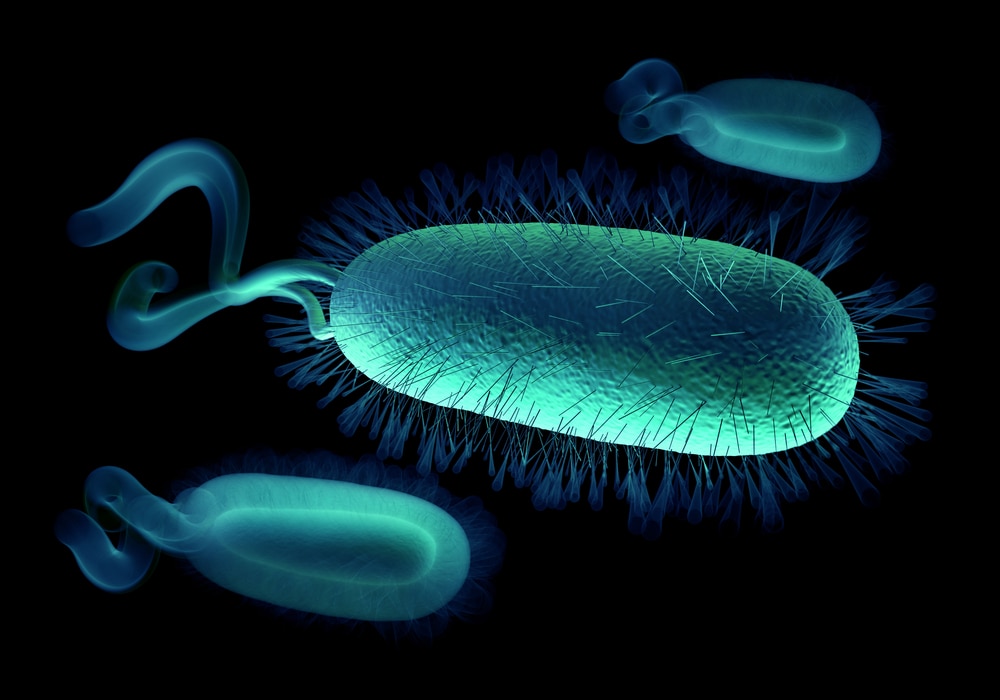
H. pylori gastritis
Helicobacter pylori (H. pylori) gastritis is one of the most common types of gastritis. Caused by infection with H. pylori bacteria, this type of gastritis is chronic and one of the most important causes of peptic ulcer disease. Without treatment for the bacterial infection, H. pylori gastritis can last a lifetime and increase the chance of developing stomach cancer.
Reactive gastropathy
Reactive gastropathy develops when the stomach lining comes into contact with irritating substances over a long period of time. Some types of pain relief medicines called nonsteroidal anti-inflammatory drugs (NSAIDs), alcohol, and bile are among the most common irritating substances. Reactive gastropathy is chronic and can be erosive. NSAIDs are the most common noninfectious cause of peptic ulcers and can cause life-threatening bleeding, obstruction, or perforation of the stomach or small intestine.
Autoimmune gastritis
Autoimmune gastritis occurs when the immune system attacks healthy cells in the stomach lining. Autoimmune gastritis is chronic and typically nonerosive.
Acute erosive gastropathy
Acute erosive gastropathy may occur after contact with irritating substances, such as NSAIDS, alcohol, or cocaine. A form of acute erosive gastropathy called stress gastritis develops when serious health problems—such as severe injuries or burns, critical illness, or sepsis—reduce the blood flow to the stomach lining. This reduced blood flow prevents the stomach’s protective mechanisms from working normally, which allows stomach acid to come into contact with and damage the stomach lining.
In acute erosive gastropathy, the stomach lining quickly develops erosions, ulcers, and bleeding. The bleeding is most often mild but may be severe.
How common are gastritis and gastropathy?
H. pylori gastritis is the most common type of gastritis, and nearly everyone who is infected with H. pylori develops chronic gastritis. About half of the world’s population is infected with H. pylori bacteria, and this infection is more common in developing countries than in developed countries.1 About 35 percent of the U.S. population is infected with H. pylori.2
Reactive gastropathy, caused by contact with irritating substances, is also relatively common, affecting about 15 percent of people in the United States.3
Other forms of gastritis and gastropathy are less common.
Who is more likely to have gastritis or gastropathy?
H. pylori infection and gastritis are more common in older people than in younger people. While the bacterial infection most often begins during childhood, H. pylori infection has become less common in the United States over time. H. pylori infection is present in about 10 to 15 percent of U.S. children younger than age 12 and in about 50 to 60 percent of U.S. adults older than age 60.1
In the United States, H. pylori infection is more common among African Americans, Hispanics/Latinos, American Indians, and Alaska Natives than among non-Hispanic whites. Compared with people born in the United States, immigrants to the United States from areas where H. pylori infection is more common, such as Asia and Central and South America, are more likely to have H. pylori.4
Reactive gastropathy is more common in people who take NSAIDs and is more common in older people than in younger people. In the United States, reactive gastropathy is present in about 2 percent of children younger than age 10 and in more than 20 percent of adults older than age 80.1
Autoimmune gastritis is more common in people who have other autoimmune disorders, including type 1 diabetes, Addison’s disease, and autoimmune thyroid diseases such as Hashimoto’s disease.
What are the complications of gastritis and gastropathy?
Peptic ulcers
Peptic ulcers are sores on the lining of your stomach or duodenum. Acute erosive gastropathy can cause peptic ulcers. H. pylori gastritis and reactive gastropathy, especially from NSAIDs, also increase your chance of developing peptic ulcers.
Anemia
H. pylori gastritis and autoimmune gastritis can cause problems absorbing iron from food, leading to iron-deficiency anemia.
Autoimmune gastritis can cause problems absorbing vitamin B12 from food. Without enough vitamin B12, the body can’t make enough healthy red blood cells, leading to pernicious anemia.
Atrophic gastritis
Chronic gastritis, most often H. pylori gastritis and autoimmune gastritis, can lead to atrophic gastritis. In atrophic gastritis, chronic inflammation leads to the loss of the glands in the stomach lining that make stomach acid and enzymes. Atrophic gastritis has also been linked to the development of stomach cancer.
Stomach cancer
Chronic H. pylori gastritis and autoimmune gastritis increase the chance of developing growths in the stomach lining. These growths may be benign or may be stomach cancer. H. pylori gastritis increases the chance of developing a type of cancer called gastric mucosa-associated lymphoid tissue (MALT) lymphoma, a type of adult non-Hodgkin lymphoma. Early diagnosis and treatment of H. pylori can prevent the development of some types of stomach cancer.
References
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.

