Intestinal Pseudo-obstruction
Return to Overview PageDefinition & Facts
In this section:
- What is intestinal pseudo-obstruction?
- Are there different types of intestinal pseudo-obstruction?
- How common is intestinal pseudo-obstruction?
- Who is more likely to have intestinal pseudo-obstruction?
- What are the complications of intestinal pseudo-obstruction?
What is intestinal pseudo-obstruction?
Intestinal pseudo-obstruction is a rare condition in which you have symptoms of intestinal obstruction, but doctors can’t find anything blocking your intestines. In intestinal pseudo-obstruction, nerve or muscle problems slow or stop the movement of food, fluid, air, and waste through your intestines.
The intestines are part of the digestive tract and are made up of the
- small intestine, which includes the duodenum, jejunum, and ileum. Most food digestion and nutrient absorption happen in your small intestine.
- large intestine, which includes the appendix, cecum, colon, and rectum. The large intestine takes in water from stool and changes stool from a liquid to a solid form.
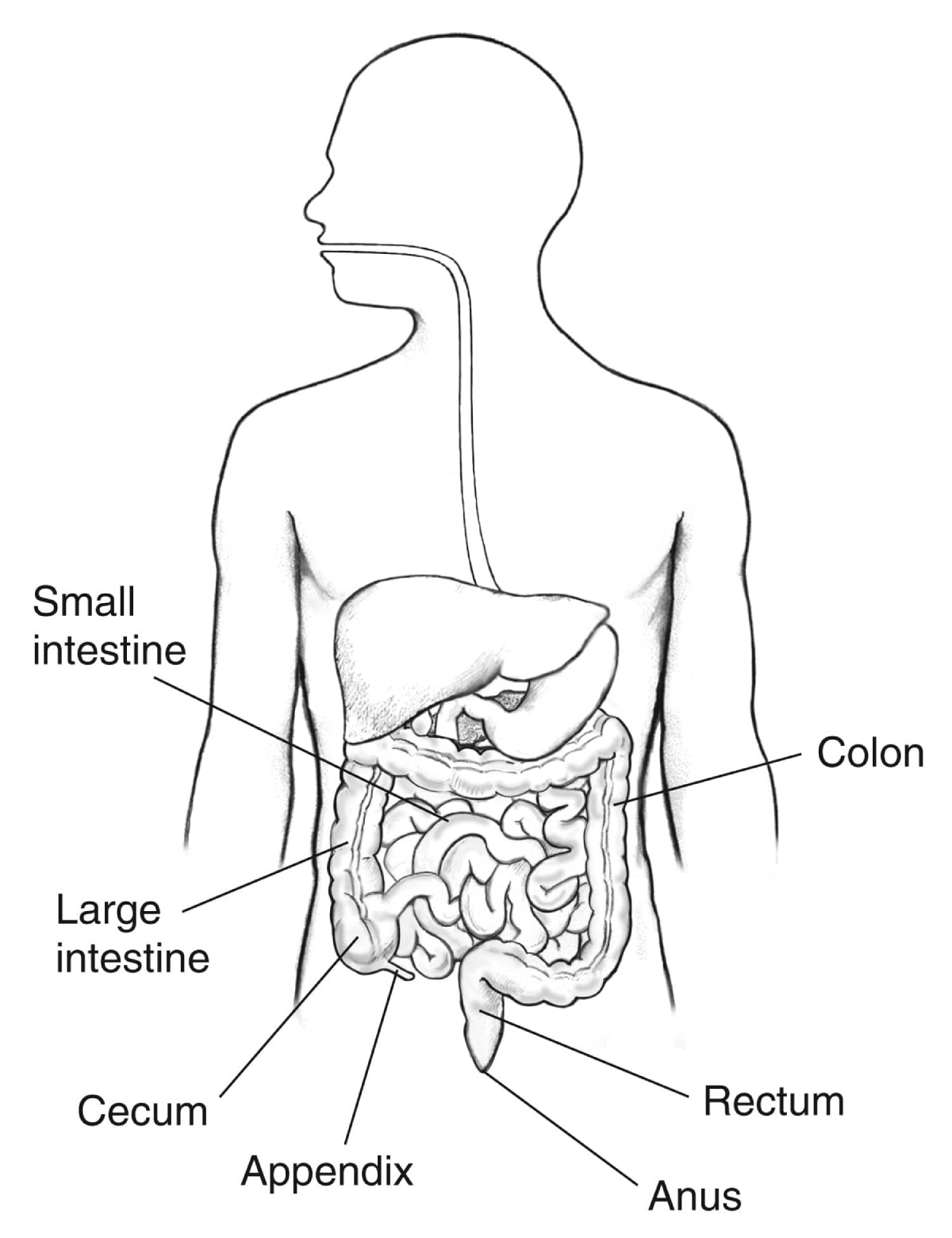 The gastrointestinal tract
The gastrointestinal tract
Are there different types of intestinal pseudo-obstruction?
The two main types of intestinal pseudo-obstruction are chronic intestinal pseudo-obstruction and acute colonic pseudo-obstruction.
Chronic intestinal pseudo-obstruction
Chronic intestinal pseudo-obstruction lasts a long time. This condition most often affects the small intestine or the colon, but it may affect other parts of the digestive tract, such as the stomach or esophagus.
Experts group chronic intestinal pseudo-obstruction into primary and secondary forms, depending on its cause.
Acute colonic pseudo-obstruction
Acute colonic pseudo-obstruction occurs suddenly and lasts a short time. This condition affects the colon. Other names for this condition include Ogilvie syndrome and colonic ileus.
How common is intestinal pseudo-obstruction?
Intestinal pseudo-obstruction is rare, and finding out how many people have it is difficult.
In the United States, research suggests that about 100 infants are born with chronic intestinal pseudo-obstruction each year.1 Research conducted in Japan found that about 8 to 10 out of every 1 million people have chronic intestinal pseudo-obstruction.1 Experts don’t know how many teens or adults experience chronic intestinal pseudo-obstruction unrelated to symptoms in infancy, or the first year of life.
Experts think that about 100 out of every 100,000 people admitted to the hospital develop acute colonic pseudo-obstruction.2
Who is more likely to have intestinal pseudo-obstruction?
Chronic intestinal pseudo-obstruction can occur in people of any age, but it most often occurs in children and young adults. In about 80% of cases, chronic intestinal pseudo-obstruction starts to cause symptoms in the first year of life.3,4
Acute colonic pseudo-obstruction is more common in older adults. The condition most often occurs in people who are hospitalized for another reason, such as severe illness, injury, or surgery.
What are the complications of intestinal pseudo-obstruction?
Chronic intestinal pseudo-obstruction and acute colonic pseudo-obstruction may lead to different complications.
Chronic intestinal pseudo-obstruction
Over time, chronic intestinal pseudo-obstruction may lead to
- malnutrition and weight loss.
- small intestinal bacterial overgrowth, an increase in the number of bacteria or a change in the type of bacteria in the small intestine. This bacterial overgrowth can affect the small intestine’s ability to absorb nutrients, including fat and fat-soluble vitamins A, D, E, and K.
- intestinal failure, which means the small intestine can’t absorb enough nutrients and water to maintain health or support growth.
Acute colonic pseudo-obstruction
Acute colonic pseudo-obstruction may cause severe swelling of the colon, which can lead to complications such as
- lack of blood flow to part of the colon.
- a perforation, or hole, in the wall of the colon. A perforation can allow the contents of the colon to spill into the abdominal cavity, which may lead to peritonitis—an infection of the lining of the abdominal cavity. Peritonitis may sometimes spread to the bloodstream, which can be life threatening.
References
Symptoms & Causes
What are the symptoms of intestinal pseudo-obstruction?
Symptoms of intestinal pseudo-obstruction vary from person to person. Symptoms may include
- abdominal pain
- bloating and feeling too full after eating a meal
- nausea and vomiting
- constipation
- diarrhea
Chronic intestinal pseudo-obstruction often causes symptoms after meals. Symptoms may be long-lasting or may come and go over time. Symptoms may be more severe at times, called acute episodes, and milder between these episodes. If chronic intestinal pseudo-obstruction affects parts of the digestive tract outside the intestines, it may cause additional symptoms. For example, if the condition affects the esophagus, it may cause problems with swallowing.
Acute colonic pseudo-obstruction symptoms may include the inability to pass stool or gas, along with the symptoms listed above. Symptoms may occur even when you don’t eat or drink.
If you or your child have symptoms of intestinal pseudo-obstruction, you should see a doctor or take your child to see a doctor right away, especially if the symptoms are severe or don’t go away. These symptoms could be a sign of either intestinal obstruction—a blockage in the intestines—or pseudo-obstruction. Without treatment, intestinal obstruction and pseudo-obstruction may lead to life-threatening complications.
What causes intestinal pseudo-obstruction?
Intestinal pseudo-obstruction occurs when nerve or muscle problems slow or stop the movement of food, fluid, air, and waste through the intestines.
Chronic intestinal pseudo-obstruction
Depending on the cause, chronic intestinal pseudo-obstruction may be primary or secondary.
Primary chronic intestinal pseudo-obstruction. Experts are still studying the causes of primary chronic intestinal pseudo-obstruction and have identified different forms of this condition.
In some forms, genes cause primary chronic intestinal pseudo-obstruction, particularly when the illness begins in the first year of life. In other forms, especially when it starts in adults, the cause is unknown. When the cause is unknown, doctors may call the condition idiopathic. People with some forms of primary chronic intestinal pseudo-obstruction also have muscle or nerve problems in other parts of the digestive tract—such as the esophagus or stomach—or, less frequently, in the urinary tract.
Most of the cases in children are primary chronic intestinal pseudo-obstruction.5
Secondary chronic intestinal pseudo-obstruction. Underlying health problems or other risk factors cause secondary chronic intestinal pseudo-obstruction. In adults, up to half of the cases of chronic intestinal pseudo-obstruction are secondary.5
A variety of health problems may cause secondary chronic intestinal pseudo-obstruction. Examples include
- diseases and disorders that affect muscles or connective tissue, such as muscular dystrophy, lupus, and scleroderma
- diseases and disorders that affect nerves, such as Parkinson’s disease and diabetic neuropathy
- endocrine disorders, such as diabetes and hypothyroidism
- health problems that affect metabolism, such as porphyria or electrolyte imbalances
- infections, such as viral infections that also cause damage to the nerves that supply the intestines, including herpes and Epstein-Barr virus
- other health problems, including celiac disease, Crohn’s disease, and some types of cancer
Other causes of secondary chronic intestinal pseudo-obstruction include
- medicines, such as opiates and antidepressants
- radiation therapy to treat cancer
- toxins—poisonous substances
Acute colonic pseudo-obstruction
Acute colonic pseudo-obstruction most often occurs in people who have a severe illness or injury or those who recently had surgery.
Health problems that may lead to acute colonic pseudo-obstruction include
- diseases and disorders that affect nerves, such as Parkinson’s disease
- heart attack, heart failure, and stroke
- infection and sepsis
- injury or physical trauma, including hip or back injury
- problems that affect metabolism, such as kidney failure, liver failure, and electrolyte imbalances
- some types of cancer, especially when cancer spreads to the area where the nerves from the spine connect with the intestines
Other factors linked to acute colonic pseudo-obstruction include
- medicines, such as opiates and antidepressants
- pregnancy, vaginal delivery, or Cesarian section
- radiation therapy to treat cancer
- surgery, such as abdominal surgery, heart surgery, organ transplantation, and joint replacement, especially knee and hip replacement
 Acute colonic pseudo-obstruction most often occurs in people who have a severe illness or injury or those who recently had surgery.
Acute colonic pseudo-obstruction most often occurs in people who have a severe illness or injury or those who recently had surgery.
References
Diagnosis
How do doctors diagnose intestinal pseudo-obstruction?
To diagnose intestinal pseudo-obstruction, the doctor will ask about symptoms, review medical and family history, perform a physical exam, and order tests.
Physical exam
During a physical exam, the doctor may
- check for bloating in the abdomen
- use a stethoscope to listen to sounds inside the abdomen
- press on the abdomen to feel for tenderness or masses
- check for signs of complications, such as fever or a fast heart rate
 To diagnose intestinal pseudo-obstruction, doctors review a patient’s history, perform a physical exam, and order tests.
To diagnose intestinal pseudo-obstruction, doctors review a patient’s history, perform a physical exam, and order tests.
What tests do doctors use to diagnose intestinal pseudo-obstruction?
Doctors may order medical tests to rule out an intestinal obstruction—a physical blockage in the intestines—and to diagnose intestinal pseudo-obstruction. Doctors may also order tests to check for causes of intestinal pseudo-obstruction.
Doctors may order different tests, depending on which type of pseudo-obstruction they think a person has.
- To diagnose chronic intestinal pseudo-obstruction, doctors may order blood tests, imaging tests such as computed tomography (CT) scans, endoscopy tests, biopsies, and other tests.
- To diagnose acute colonic pseudo-obstruction, doctors most often order blood tests and imaging tests, such as x-rays of the abdomen or CT scans.
Blood tests
For a blood test, a health care professional will take a blood sample and send the sample to a lab. Doctors may order blood tests to help find the cause of pseudo-obstruction or to check for complications.
Imaging tests
Doctors may order imaging tests, including
- x-rays, which use a small amount of radiation to create pictures of the inside of the body
- CT scans, which use a combination of x-rays and computer technology to create images
- magnetic resonance imaging (MRI), which takes pictures of the body’s internal organs and soft tissues without using x-rays
- upper GI series, which uses x-rays and water-soluble contrast medium—a special liquid that makes the digestive tract easier to see on x-rays—to view the upper GI tract, including the small intestine
- lower GI series, which uses x-rays and water-soluble contrast medium to view the lower GI tract
Endoscopy tests
Doctors may order endoscopy tests to help diagnose chronic intestinal pseudo-obstruction. During an endoscopy, doctors use an endoscope—a long, flexible, narrow tube with a light and tiny camera on one end—to view inside the digestive tract. Two types of endoscopy tests are
- upper GI endoscopy, which doctors use to see inside the upper GI tract
- colonoscopy, which doctors use to see inside the lower GI tract
Doctors may take biopsies during endoscopy tests.
Biopsies
To help diagnose chronic intestinal pseudo-obstruction, doctors may take biopsies—small pieces of tissue—from the digestive tract lining or intestinal wall.
A doctor may take biopsies during an endoscopy test by passing an instrument through the endoscope to take a small piece of tissue. In some cases, doctors may perform surgery to take biopsies of the intestinal wall. If a patient is having surgery to treat chronic intestinal pseudo-obstruction, doctors may take biopsies during the surgery. Biopsies of the intestinal wall may help doctors find the cause of chronic intestinal pseudo-obstruction.
A pathologist will examine the biopsy tissue under a microscope to check for signs of chronic intestinal pseudo-obstruction or health problems that could cause pseudo-obstruction.
Other tests
Doctors may order additional tests to find out how well the digestive tract is working. These tests can help diagnose chronic intestinal pseudo-obstruction, find the cause, or guide treatment. Examples include
- scintigraphy tests. These tests involve eating a meal with a small dose of a radioactive substance. Doctors use special computers and external cameras to track the substance as it passes through the digestive tract.
- manometry tests. These tests measure muscle pressure and movements in part of the digestive tract, such as the esophagus, small intestine, colon, or rectum and anus.
- gastric emptying breath test. This test involves eating a meal that contains a substance that is absorbed in the intestines and is eventually passed into the breath. After a person eats the meal, a health care professional collects samples of his or her breath over a period of a few hours. The test can show how fast the stomach empties by measuring the amount of the substance in the breath.
Treatment
How do doctors treat intestinal pseudo-obstruction?
Doctors recommend different treatments for chronic intestinal pseudo-obstruction and acute colonic pseudo-obstruction.
Chronic intestinal pseudo-obstruction
Doctors treat chronic intestinal pseudo-obstruction with nutrition support, medicines, decompression, and sometimes surgery. If an underlying health problem is causing chronic intestinal pseudo-obstruction, doctors will also treat the underlying health problem as needed.
Nutrition support. People with chronic intestinal pseudo-obstruction may have problems getting enough nutrients from their food and drinks. Doctors may recommend diet changes to help prevent malnutrition and weight loss. Doctors often recommend a diet low in fat and uncooked fiber.
However, people who can’t get enough nutrients from their diet may need nutrition support. Nutrition support may include
- enteral nutrition, in which a person receives liquid food through a tube inserted into the stomach or small intestine. The tube may be inserted through the nose, or it may be inserted through the wall of the abdomen during surgery or with the help of endoscopy.
- parenteral nutrition, in which a person receives nutrients through an intravenous (IV) tube, which is a tube inserted into a vein.
Parenteral nutrition may lead to serious complications, such as blood clots in veins or infections. Doctors only recommend parenteral nutrition if a person can’t get enough nutrients from their diet or from enteral nutrition.
 People who aren’t able to get enough nutrients from their diet may need nutrition support.
People who aren’t able to get enough nutrients from their diet may need nutrition support.
Medicines. Doctors may prescribe medicines to help relieve the symptoms of chronic intestinal pseudo-obstruction, including
- medicines that help food move through the digestive tract more quickly.
- medicines that help relieve nausea and vomiting.
- antibiotics, which doctors may prescribe to treat small intestinal bacterial overgrowth.
- pain medicines, if needed. Doctors may recommend avoiding pain medicines, such as opioids, that slow down food moving through the digestive tract and may worsen the pseudo-obstruction.
Decompression. Decompression means removing gas and fluids from the digestive tract to relieve pressure and symptoms of pseudo-obstruction. To decompress the digestive tract, doctors may
- insert a tube through the nose and into the stomach
- perform a colonoscopy
- perform surgery
Surgery. In some cases, doctors recommend surgery to treat chronic intestinal pseudo-obstruction. Types of surgery include
- gastrostomy or jejunostomy, in which doctors place a tube from outside your body through the abdominal wall, directly into the stomach or small intestine. The tube can be used for enteral nutrition and for decompression.
- ileostomy or colostomy, which may help with decompression.
- bowel resection, or surgery to remove part of the intestine, which doctors recommend rarely, usually when imaging tests show the pseudo-obstruction affects only a segment of the intestine.
- intestinal transplant, which doctors may recommend for people who require parenteral nutrition but cannot start or continue parenteral nutrition safely.
Acute colonic pseudo-obstruction
Doctors most often treat acute colonic pseudo-obstruction with an approach called conservative management. In some cases, other treatments may be needed.
Conservative management. Doctors may treat acute colonic pseudo-obstruction with conservative management if you are not likely to have or develop complications. As part of conservative management, doctors typically
- stop any medicines that could worsen the pseudo-obstruction, especially opioid pain medicines
- treat any infections or other health problems
- instruct you not to eat or drink anything because pseudo-obstruction will stop the movement of food, fluid, air, and waste through your intestines
- give you IV fluid and electrolytes as needed
- give you medicine to help relieve the pseudo-obstruction
- insert tubes into your stomach or rectum to decompress your digestive tract
- encourage you to walk if you can
 As part of conservative management for acute colonic pseudo-obstruction, doctors typically encourage you to walk if you can.
As part of conservative management for acute colonic pseudo-obstruction, doctors typically encourage you to walk if you can.
Other treatments. If acute pseudo-obstruction doesn’t improve with conservative management in 2 or 3 days, doctors may recommend other treatments.6 Doctors may also recommend other treatments if you have, or are likely to develop, complications. Other treatments may include
- medicine to help relieve the pseudo-obstruction.
- a colonoscopy to decompress the colon. In some cases, during colonoscopy, doctors place a tube in the colon and leave it there for a few days to help with decompression. The tube will eventually pass naturally.
- surgery to decompress the colon or to remove part of the colon damaged by complications, particularly perforation.
References
Eating, Diet, & Nutrition
What should I eat if I have intestinal pseudo-obstruction?
Doctors may recommend diet changes for people who have intestinal pseudo-obstruction.
Chronic intestinal pseudo-obstruction
For people who have chronic intestinal pseudo-obstruction, diet changes may help reduce symptoms and prevent complications, such as malnutrition, weight loss, and small intestinal bacterial overgrowth.
Doctors may recommend
- a diet low in fat, fiber, lactose, and fructose
- cooking all vegetables and passing them through a blender to make them easier to digest
- eating five or six small meals per day
- liquid meals and dietary supplements
- vitamin supplements
For safety reasons, talk with your doctor before using dietary supplements or any other complementary or alternative medicines or practices.
People who aren’t able to get enough nutrients from their diet may need nutrition support. Nutrition support may include enteral nutrition or parenteral nutrition.
 Doctors may recommend diet changes for people who have chronic intestinal pseudo-obstruction.
Doctors may recommend diet changes for people who have chronic intestinal pseudo-obstruction.
Acute colonic pseudo-obstruction
As part of conservative management for acute colonic pseudo-obstruction, your doctor may instruct you not to eat or drink anything for a short time. Health care professionals will give you intravenous (IV) fluids and electrolytes as needed.
Clinical Trials
The NIDDK conducts and supports clinical trials in many diseases and conditions, including digestive diseases. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for intestinal pseudo-obstruction?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of intestinal pseudo-obstruction. For example, studies seek to
- better understand chronic intestinal pseudo-obstruction and other rare intestinal disorders
- find new treatments for intestinal pseudo-obstruction
- find new ways to examine how well the digestive tract is working
Find out if clinical studies are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies for intestinal pseudo-obstruction are looking for participants?
You can find clinical studies on intestinal pseudo-obstruction at ClinicalTrials.gov. In addition to searching for federally funded studies, you can expand or narrow your search to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank:
Michael Camilleri, M.D., Mayo Clinic

