Urinary Retention
Return to Overview PageDefinition & Facts
In this section:
- What is urinary retention?
- How common is urinary retention?
- Who is more likely to develop urinary retention?
- What are the complications of urinary retention?
What is urinary retention?
Urinary retention is a condition in which you are unable to empty all the urine from your bladder. Urinary retention is not a disease, but a condition that may be related to other health problems, such as prostate problems in men or a cystocele in women. Urinary retention can be acute—a sudden inability to urinate at all, or chronic—a gradual inability to empty the bladder.
Acute urinary retention
Acute urinary retention happens suddenly and lasts only a short time. People with acute urinary retention are unable to urinate even though they have a full bladder.
Acute urinary retention can cause severe pain and be life threatening. If you are suddenly unable to urinate, it’s important that you seek emergency medical treatment right away.
Chronic urinary retention
Chronic urinary retention develops over time. People with chronic urinary retention can urinate but cannot completely empty the urine from their bladders. Many people with chronic urinary retention do not know they have the condition because they may not experience any symptoms.
How common is urinary retention?
Acute urinary retention is common in older men, and the likelihood of experiencing acute urinary retention increases with age. Over a five-year period, approximately 1 in 10 men over the age of 70 and almost one in three men in their 80s will develop acute urinary retention.1
Acute urinary retention is much less common in women. Each year, about 3 in 100,000 women develop acute urinary retention.1 Acute urinary retention in children is rare.
Researchers aren’t sure how common chronic urinary retention is. However, researchers do know that chronic urinary retention affects older men more than any other group.
Who is more likely to develop urinary retention?
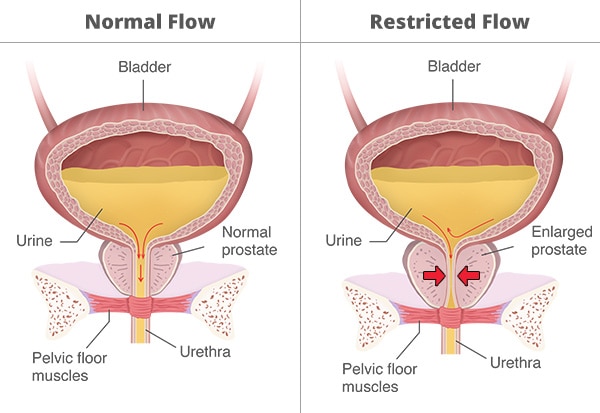
Urinary retention affects both men and women, but it occurs more often in men, especially as they get older. Men who have benign prostatic hyperplasia (BPH)—a condition in which the prostate gland is enlarged—are more likely to develop urinary retention. As the prostate enlarges, it pushes against the urethra, blocking the flow of urine out of the bladder. BPH is a common prostate problem for men older than age 50.
What are the complications of urinary retention?
People who have urinary retention may have complications, including
- Urinary tract infection. When your urinary tract is emptying completely, bacteria that normally enter your urinary tract are flushed out when you urinate. With urinary retention, your urine doesn’t completely flow out, which allows the normally harmless bacteria a chance to multiply and infect your urinary tract. Serious problems can occur if the infection spreads to your kidneys.
- Bladder damage. If urinary retention is not treated, your bladder may become stretched too far or for long periods. When stretched too far or for too long, the muscles in your bladder may become damaged and no longer work correctly.
- Kidney damage. Your urinary tract is designed to have the urine flow from the kidneys, through the ureters, to the bladder, and out the urethra. When you have urinary retention, you aren’t able to empty the urine from your bladder and the urine may back up into your kidneys. Your kidneys can become so full of urine that they swell and press on nearby organs. This pressure can damage your kidneys and in some cases may lead to chronic kidney disease and kidney failure.
- Urinary incontinence. When your bladder does not fully empty, it can lead to you leaking urine, called overflow incontinence.
Working with a health care professional to prevent and treat these complications is important for both the health of your urinary tract and your overall health.
Reference
Symptoms & Causes
What are the symptoms of urinary retention?
Acute urinary retention
Symptoms of acute urinary retention may include
- the inability to urinate
- pain—often severe—in your lower abdomen
- the urgent need to urinate
- swelling of your lower abdomen
Chronic urinary retention
Chronic urinary retention develops over time and may cause few or no symptoms, which may make it hard to detect. If your chronic urinary retention causes symptoms, they may include
- the inability to completely empty your bladder when urinating
- frequent urination in small amounts
- difficulty starting the flow of urine, called hesitancy
- a slow urine stream
- the urgent need to urinate, but with little success
- feeling the need to urinate after finishing urination
- leaking urine without any warning or urge
- lower abdominal pain or discomfort
 The symptoms of acute urinary retention are often severe and can include abdominal pain and the inability to urinate, whereas chronic urinary retention may cause few or no symptoms.
The symptoms of acute urinary retention are often severe and can include abdominal pain and the inability to urinate, whereas chronic urinary retention may cause few or no symptoms.
When should I see a health care professional?
See a health care professional right away if you are unable to urinate or have severe pain in your abdomen. Acute urinary retention can be life threatening.
If you have any of the other symptoms of urinary retention, such as trouble urinating, frequent urination, or leaking urine, talk with your health care professional about your symptoms and possible treatments. Chronic urinary retention can cause serious health problems.

What causes urinary retention?
The causes of urinary retention are related to either a blockage that partially or fully prevents urine from leaving your bladder or urethra, or your bladder not being able to maintain a strong enough force to expel all the urine.
Blockage or narrowing in the urethra or bladder neck
For you to be able to urinate normally, all parts of your urinary tract need to work together in the correct order. Urine normally flows from your kidneys, through the ureters to your bladder, and out the urethra. If a blockage or narrowing occurs somewhere along the urinary tract, you may have difficulty urinating, and if the blockage is severe, you may not be able to urinate at all.
Medical problems that may narrow the urethra and block urine flow include
- enlarged prostate, or benign prostatic hyperplasia
- bladder outlet obstruction, such as urethral stricture or scar tissue in the bladder neck
- pelvic organ prolapse, including cystocele and rectocele
- urinary tract stones, also called calculi
- constipation
- pelvic masses, such as noncancerous or cancerous tumors, fibroids, polyps, or clots
- tight pelvic floor muscles
- infections, such as urinary tract infection, sexually transmitted diseases, or prostatitis
- trauma to the pelvis, urethra, or penis
Inefficient bladder contraction (underactive bladder)
You may develop urinary retention when your bladder muscles aren’t able to contract with enough strength or do not contract long enough to empty your bladder completely—also called underactive bladder. Causes of underactive bladder include
Neurological problems. Urinary retention can occur when there is a problem with your nervous system that prevents messages from travelling from your brain to your bladder and urethra. There are many different causes of neurological problems, including
- Parkinson’s disease
- multiple sclerosis
- Alzheimer’s disease
- stroke
- birth defects, such as spina bifida
- diabetes
- spinal cord injury
- traumatic brain injury
- pelvic injury
- vaginal birth
- Guillain-Barré syndrome
- Fowler’s syndrome
- heavy metal poisoning
Medicines. Urinary retention can be caused by certain medicines that interfere with nerve signals to your bladder, urethra, or prostate. Examples of these medicines include
- alpha-adrenergic agonists
- anticholinergics and antispasmodics
- antidepressants
- antihistamines and decongestants
- antiparkinsonian medications
- antipsychotics
- benzodiazepines
- calcium channel blockers
- nonsteroidal anti-inflammatory drugs, such as aspirin and ibuprofen
- opioids
- serotonin and noradrenaline reuptake inhibitors
Surgery. It is common to develop temporary urinary retention right after surgery. During surgery, you are often given intravenous (IV) fluid, which may lead to a full bladder. You are also given anesthesia, which can prevent you from feeling the need to urinate despite having a full bladder. In addition, pelvic surgery can cause swelling, scar tissue, and trauma that can partially or fully block the flow of urine out of your bladder or urethra.
Weak bladder muscles. Bladder muscles that are weak may not contract with enough strength or force to empty the bladder completely. Causes of weakness can include
- age-related loss of bladder muscle strength
- overdistention—a bladder that has been stretched such that the muscles are damaged
- pregnancy and childbirth
- trauma
Diagnosis
How do health care professionals diagnose urinary retention?
Health care professionals use your medical history, a physical exam, and a postvoid residual urine measurement to diagnose urinary retention. Your health care professional may also order lab and other diagnostic tests to help find the cause of your urinary retention.
Medical history
A health care professional will record your medical history and may ask about your
- symptoms, also sometimes called lower urinary tract symptoms
- current and past medical problems such as operations and use of a catheter
- prostate problems
- pregnancy and childbirth history
- over-the-counter and prescription medicines
- eating and drinking habits
- bowel habits
Physical exam
Your health care professional will perform a physical exam, including a check of your lower abdomen, a rectal exam, and a neurological evaluation. If you’re a woman, the health care professional will also perform a pelvic exam.
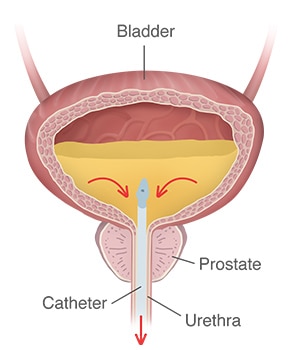
Postvoid residual urine measurement
Health care professionals use a postvoid residual measurement to find out how much urine is left in the bladder after urination. The remaining urine is called the postvoid residual. Your health care professional will use a catheter or ultrasound equipment to measure the postvoid residual urine.

Lab tests
Your health care professional may order the following lab tests to look for signs of certain diseases and conditions that may be causing your urinary retention.
- Urinalysis is used to find medical conditions that may be causing urinary retention, such as a urinary tract infection (UTI), a kidney problem, or diabetes.
- Blood tests are used to show problems with kidney function or a chemical imbalance in your body.

Imaging tests
Your health care professional may use the following urinary tract imaging tests to diagnose other conditions that may be causing your urinary retention.
- Ultrasound is a type of imaging that uses sound waves to look at structures inside the body without exposing you to radiation.
- Voiding cystourethrogram (VCUG) uses x-rays to show how urine flows through the bladder and urethra.
- Magnetic resonance imaging (MRI) uses magnets and radio waves to make pictures of the urinary tract and spine.
- Computed tomography (CT) scan uses a combination of x-rays and computer technology to create images of your urinary tract.

Urodynamic testing
Urodynamic testing is a group of tests that look at how well the bladder, sphincters, and urethra are storing and releasing urine. Your health care professional may use the following urodynamic tests to help diagnose urinary retention.
- Uroflowmetry measures the amount of urine released from your body and how quickly the urine comes out.
- Pressure flow studies measure the pressure in your bladder and the flow rate as you urinate.
- Video urodynamics takes pictures and videos of your bladder as it fills and empties.
- Cystometry measures how much urine your bladder can hold, how much pressure builds up in your bladder as it stores urine, and how full your bladder is when you begin to feel the urge to urinate.
- Electromyography measures how well your muscles respond to your nerves in and around your bladder and sphincters.
Cystoscopy
A cystoscopy is a procedure that uses a cystoscope—a long, thin instrument—to look inside your urethra and bladder. The health care professional will look for swelling, redness, signs of infection, cancer, and structural problems.
Treatment
How do health care professionals treat urinary retention?
Health care professionals treat urinary retention based on the type of urinary retention—acute or chronic—and the cause of the urinary retention.
Draining the bladder
With acute urinary retention, a health care professional will immediately drain the urine from your bladder using a catheter. Removing the urine from the bladder eases your pain and helps prevent your bladder and kidneys from being damaged.
If you have chronic urinary retention, your health care professional will first try to diagnose and treat the cause of your retention. However, your health care professional may need to use a catheter to drain the urine from your bladder if the retention continues or becomes severe.
In some cases, people with urinary retention need to continue using a catheter to drain urine from the bladder until their urinary retention can be fixed. The catheter can be indwelling—left in your bladder for a short or long time, or intermittent—inserted to drain the bladder when needed and then removed. If you have to use an intermittent catheter, a health care professional can teach you how to use the catheter.
Medicines
Your health care professional may suggest that you take medicine to help treat the medical condition causing your urinary retention
- 5-alpha reductase inhibitors help to stop the growth of or shrink the prostate, which can improve the flow of urine. Examples include dutasteride and finasteride.
- Alpha-blockers treat the symptoms of prostate enlargement (benign prostatic hyperplasia) by relaxing muscles in the bladder neck and prostate, which makes it easier to urinate. Examples include alfuzosin, doxazosin, prazosin, silodosin, tadalafil, tamsulosin, and terazosin.
- A combination of a 5-alpha-reductase inhibitor and an alpha-blocker, such as finasteride and doxazosin or dutasteride and tamsulosin, may work better than an individual medicine alone.
- Antibiotics treat infections that may cause urinary retention, such as urinary tract infections and prostatitis.
In some people, certain medicines may cause urinary retention. If your health care professional thinks that a medicine is causing your urinary retention, you may be asked to lower the dose or stop using the medicine.
All medicines, even over-the-counter medicines, have side effects. Always consult a health care professional before using any medicine for more than a few days.
Medical procedures and devices
Your health care professional may recommend a medical procedure or device to treat your urinary retention, depending on the cause of the retention. Examples of these procedures and devices include
- cystoscopy—using a cystoscope to look inside the urethra and bladder to find and remove blockages such as urinary tract stones
- laser therapy—therapy that uses a strong beam of light to treat an area of enlarged prostate tissue by breaking up the blockage and reducing the obstruction
- prostatic urethral lift, or UroLift—using tiny implants to lift and hold the prostate away from the urethra so urine can flow more freely
- transurethral electrovaporization—a procedure that uses heat to vaporize an area of enlarged prostate tissue
- transurethral water vapor therapy, or Rezum—therapy that uses water vapor, or steam, to shrink an enlarged prostate
- urethral dilation—gradually increasing the size of the urethral opening by stretching the scar tissue, to help treat urethral stricture
- vaginal pessary—a stiff ring that is inserted into the vagina to help stop urine leakage, such as with cases of a cystocele (prolapsed bladder) or rectocele
Surgery
Your health care professional may consider surgery to help treat the cause of your urinary retention if other less invasive treatments don’t work. Some of these treatments may include
- removing part of the prostate
- repairing urethral strictures or bladder neck scar tissue
- repairing pelvic organ prolapse
- removing a tumor, abnormal uterus, or damaged portion of a herniated disc
- repairing an abnormal bladder
- performing a urinary diversion procedure to reroute the normal flow of urine out of your body
How can I treat my urinary retention?
Your health care professional may recommend you try self-care treatments—either alone or in addition to other treatments—to manage your urinary retention.
Do physical therapy
Your health care professional may suggest that you work with a physical therapist who specializes in pelvic floor problems. The physical therapist will work to stretch tight pelvic floor muscles and help you keep them relaxed. Pelvic floor muscle exercises, also called Kegel exercises, help the nerves and muscles that you use to empty your bladder work better.

Train your bladder
Your health care professional may suggest timed voiding—urinating at set times—to help prevent your bladder from becoming too full. Another bladder training technique that your health care professional may recommend is double voiding—waiting a short time after you urinate to try and go again—to help make sure your bladder is completely empty after you urinate.
Take extra time in the bathroom to relax and empty the bladder completely. Women should try to relax the muscles around their bladder when they urinate to make it easier to go. It’s best to sit on the toilet seat or in a full crouching squat. Hovering over a toilet seat to avoid touching it does not allow muscles to fully relax and may result in urine being left in the bladder.
Prevention
Can I prevent urinary retention?
You can’t always prevent urinary retention, but you can take steps to lower your chances of developing the condition.
Change your bathroom habits
Use the bathroom whenever you have an urge to go. Often, people hold their urine because it’s not a good time to go to the bathroom. However, regularly holding urine in can wear out your bladder muscles. You’re also more likely to develop a urinary tract infection (UTI) if you hold urine in. UTIs can cause urinary retention.

Stay in tune with your body
Pay attention to how often you feel the urge to urinate. If it becomes easier to delay using the bathroom and you stretch out the time between urinating, you may gradually stretch out your bladder. Also note if it becomes more difficult for you to begin to urinate or you feel that you’re not able to completely empty your bladder. These may be early signs of urinary retention.
Be aware of any changes to your urination habits after surgery or a serious back injury. It’s common for urinary retention to develop—either immediately or over time—after having surgery or injuring your back.
Talk with your health care professional if you notice any of the signs of urinary retention. You may be able to prevent the condition from becoming more severe if you get help early on.
Take medicine as prescribed
Men with prostate problems, such as benign prostatic hyperplasia, should take the medicines prescribed by their health care professional and avoid medicines that may lead to urinary retention, such as decongestants and nonsteroidal anti-inflammatory drugs.
Do pelvic floor muscle exercises
Pelvic floor exercises, also called Kegel exercises, can make the pelvic floor muscles stronger and improve bladder and bowel function. Both men and women can benefit from pelvic floor muscle exercises.
Make dietary and lifestyle modifications
You can help prevent urinary retention caused by constipation by making changes to your diet and lifestyle. To help prevent constipation, get enough fiber in your diet, drink plenty of water and other liquids, and get regular physical activity.

Clinical Trials
The NIDDK conducts and supports clinical trials in many diseases and conditions, including urologic disease. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for urinary retention?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help health care professionals and researchers learn more about disease, and improve health care for people in the future.
Researchers are studying many aspects of urinary retention, such as
- improved understanding of the causes of urinary retention and identifying the causes earlier
- new treatments for this condition
- preventing urinary retention after surgery
- strategies for improving catheter management
Find out if clinical studies are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies for urinary retention are looking for participants?
You can view a filtered list of clinical studies on urinary retention that are open and recruiting at ClinicalTrials.gov. You can expand or narrow the list to include clinical studies from industry, universities, and individuals; however, the NIH does not review these studies and cannot ensure they are safe. Always talk with your health care professional before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank
Steven A. Kaplan, M.D., Icahn School of Medicine at Mount Sinai

