Proctitis
Return to Overview PageDefinition & Facts
In this section:
- What is proctitis?
- Are there different types of proctitis?
- How common is proctitis?
- Who is more likely to develop proctitis?
- What are the complications of proctitis?
What is proctitis?
Proctitis is inflammation of the lining of your rectum. The rectum is the lower end of the large intestine.
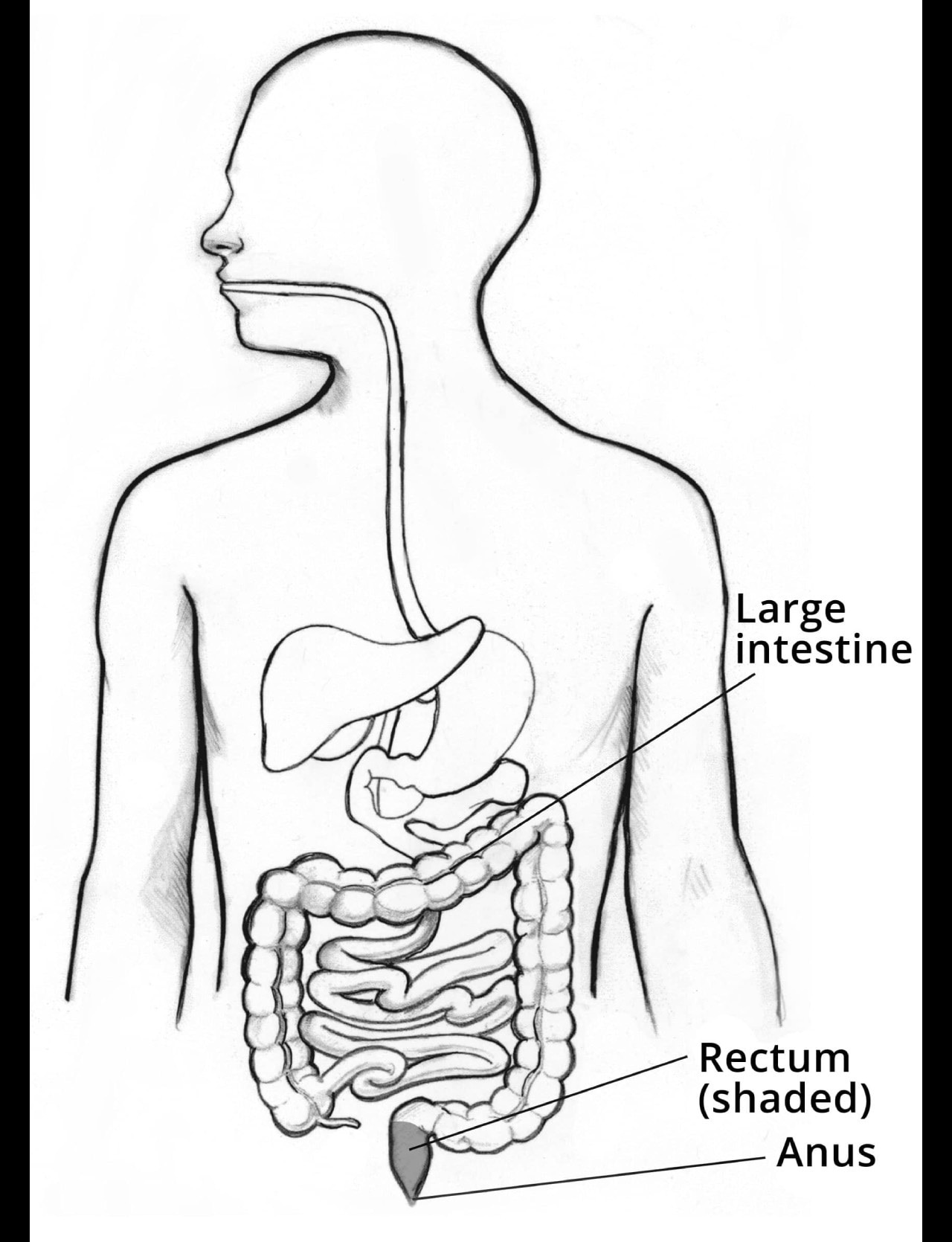 The digestive system, showing the location of the large intestine, rectum, and anus.
The digestive system, showing the location of the large intestine, rectum, and anus.
Are there different types of proctitis?
Experts have identified several types of proctitis, which have different causes and treatments.
Proctitis may be chronic or acute. Chronic proctitis can last a long time or may come and go over time. Acute proctitis develops suddenly and lasts a short time.
Common types of proctitis include the following.
Proctitis in IBD
Proctitis may be part of inflammatory bowel disease (IBD). Ulcerative colitis and Crohn’s disease are common types of IBD that may cause proctitis. Proctitis in IBD is chronic, and it is the most common type of proctitis.1
Infectious proctitis
Certain infections, including some types of sexually transmitted diseases (STDs) and food poisoning, may cause proctitis. Infectious proctitis is most often acute.
Radiation proctitis or radiation proctopathy
Radiation proctitis is a commonly used term for a condition that is also called radiation proctopathy. This condition may occur after a person receives radiation therapy to treat cancer or other diseases in the pelvic area or lower abdomen. Radiation proctopathy may be acute or chronic.
Acute radiation proctopathy most often occurs within 3 months of starting radiation therapy.2 Acute radiation proctopathy typically lasts a short time, but it may become chronic.
Chronic radiation proctopathy most often begins 9 to 14 months after radiation therapy.3 However, the condition may develop many years after radiation therapy has ended.
Diversion proctitis
Diversion proctitis is inflammation of the rectum that may develop after ostomy surgery of the bowel, also called bowel diversion. After ostomy surgery, waste leaves your body through an opening called a stoma in your abdominal wall instead of passing through the rectum and anus.
Diversion proctitis is chronic and most often starts 3 months to 3 years after ostomy surgery.2
How common is proctitis?
Experts don’t know how common all types of proctitis are. However, researchers have studied how common specific types of proctitis are in certain groups of people. For example
- About 30% of people diagnosed with ulcerative colitis have inflammation in the rectum only.2 Doctors call this condition ulcerative proctitis.
- Among people who have radiation therapy to treat cancer in the pelvic area or lower abdomen, about 75% develop acute radiation proctopathy and up to 20% develop chronic radiation proctopathy.4
- Among people who don’t have the rectum removed during ostomy surgery, inflammation in the rectum—called diversion proctitis—is common. However, less than half of these people develop symptoms.2
Who is more likely to develop proctitis?
You are more likely to develop proctitis if you
- have ulcerative colitis or Crohn’s disease
- have a sexually transmitted disease or engage in anal sex
- had radiation therapy to your pelvic area or lower abdomen to treat certain types of cancer
- had ostomy surgery of the bowel and did not have your rectum removed
What are the complications of proctitis?
If your proctitis isn’t treated or doesn’t get better with treatment, you may develop complications, including
- abscesses—painful, swollen, pus-filled areas caused by infection
- chronic or severe bleeding that can lead to anemia
- fistulas—an abnormal passage, or tunnel, between two organs or between an organ and the outside of the body
- rectal stricture—an abnormal narrowing of your rectum
- ulcers—sores in the lining of your rectum
References
Symptoms & Causes
What are the symptoms of proctitis?
Common symptoms of proctitis include
- tenesmus, which means feeling a constant urge to have a bowel movement even though your bowel may be empty
- an urgent need to have a bowel movement
- diarrhea or constipation
- cramping and pain in your anus, rectum, or the left side of your abdomen, which may occur during bowel movements
- passing blood with your stool or rectal bleeding
- passing mucus or pus with your stool
If you pass blood, mucus, or pus from your rectum or have severe abdominal pain, you should see a doctor right away.
What causes proctitis?
Different types of proctitis have different causes.
Common causes of proctitis
Proctitis of inflammatory bowel disease. Two types of inflammatory bowel disease—ulcerative colitis and Crohn’s disease—may cause proctitis.
- Ulcerative colitis causes inflammation and ulcers in the large intestine, including the rectum.
- Crohn’s disease may cause inflammation and irritation of any part of the digestive tract. When it affects the rectum, it can cause proctitis.
Infectious proctitis. Several sexually transmitted diseases (STDs) can infect the rectum and cause proctitis, including
Other infections in the rectum that can cause proctitis include
- infections that cause food poisoning, such as Salmonella, Shigella, and Campylobacter infections
- Clostridioides difficile (C. diff) infection, which most often occurs while a person is taking antibiotics or shortly thereafter
 Shigella, Campylobacter, and Salmonella bacteria
Shigella, Campylobacter, and Salmonella bacteria
Radiation proctitis or radiation proctopathy. Radiation therapy to treat cancer in your pelvic area or lower abdomen may cause radiation proctopathy. People may develop radiation proctopathy after receiving radiation therapy to treat many types of cancer, including cervical, prostate, and rectal cancer.
In radiation proctopathy, the lining of your rectum is damaged. Unlike other types of proctitis, radiation proctopathy involves little or no inflammation, and this is why experts prefer the term proctopathy instead of proctitis.
Diversion proctitis. People who don’t have their rectum removed during ostomy surgery of the bowel may develop diversion proctitis, or inflammation in the remaining rectum. Surgeons create an ostomy—or stoma—by bringing part of your intestine through your abdominal wall. After surgery, waste leaves your body through the stoma in your abdominal wall instead of passing through your rectum and anus.
Experts aren’t sure why some people develop diversion proctitis after ostomy surgery. However, the condition typically goes away after a second surgery to close the ostomy and reconnect your rectum to the rest of your intestines.
Other causes of proctitis
Other factors may cause proctitis. These include
- injury to the anus or rectum
- side effects of medicines, such as nonsteroidal anti-inflammatory drugs (NSAIDs)
- lack of blood flow to the rectum
Diagnosis
How do doctors diagnose proctitis?
Doctors will ask about your medical history, perform a physical exam, and order tests to diagnose proctitis and find the cause.
Medical history
Your doctor will review your symptoms and ask about your medical history, including
- current and past medical conditions
- family history of digestive diseases, such as inflammatory bowel disease (IBD)
- history of radiation therapy for cancer
- history of, or risk factors for, sexually transmitted diseases (STDs)
- history of travel to areas where some infections that cause proctitis are more common
- use of medicines, including antibiotics or nonsteroidal anti-inflammatory drugs (NSAIDs)
 Your doctor will review your symptoms and ask you about your medical history.
Your doctor will review your symptoms and ask you about your medical history.Physical exam
Your doctor will perform a physical exam, which may include a digital rectal exam, to check for signs of proctitis or other problems in the rectum.
What tests do doctors use to diagnose proctitis?
Blood tests
A health care professional will take a blood sample from you and send it to a lab. Blood tests can show signs of infections or other conditions that may cause proctitis.
Stool tests
A doctor will give you a container for catching and storing stool. You will receive instructions on where to send or take the container for analysis. Stool tests may show signs of infections that can cause proctitis.
Rectal cultures
A doctor will use a cotton swab to collect a sample of the bacteria and other microbes inside your rectum. A rectal culture can show signs of infections that cause proctitis.
Endoscopy
A doctor uses an endoscope—a long, flexible, narrow tube with a light and tiny camera on one end—to view the lining of your anus, rectum, and colon. The doctor may pass a tool through the endoscope to take biopsies of the lining of your rectum and colon. A pathologist will examine the biopsied tissue under a microscope.
Common endoscopy procedures that doctors can use to diagnose, find the cause, and check for complications of proctitis include
- colonoscopy to view the lining of your rectum and your entire colon
- flexible sigmoidoscopy to view the lining of your rectum and lower colon
Doctors may also view the inside of your anus or rectum with a shorter, rigid scope, such as a proctoscope or anoscope.
 Doctors may use endoscopy tests to diagnose proctitis.
Doctors may use endoscopy tests to diagnose proctitis.
Treatment
How do doctors treat proctitis?
Your doctor will recommend treatments based on the type of proctitis you have and its cause.
Proctitis in IBD
Doctors prescribe medicines to treat proctitis due to inflammatory bowel disease (IBD)—ulcerative colitis or Crohn’s disease. Medicines may reduce inflammation in the rectum and help bring on and maintain IBD remission—a time when your symptoms disappear.
Medicines to treat proctitis in IBD include
- aminosalicylates
- corticosteroids, also called steroids
- immunosuppressants
- biologics
Doctors may recommend surgery to treat proctitis in IBD if medicines don’t work or if you develop complications.
 Doctors prescribe medicines to treat proctitis in IBD.
Doctors prescribe medicines to treat proctitis in IBD.
Infectious proctitis
Doctors typically prescribe medicines, such as antibiotics to treat bacterial infections or antiviral medicines to treat viral infections.
Radiation proctitis or radiation proctopathy
Doctors treat radiation proctopathy based on how severe your symptoms are. If you have mild symptoms, your doctor may recommend medicines to help reduce symptoms and heal the lining of your rectum.
If radiation proctopathy causes rectal bleeding that is severe or doesn’t stop, doctors may use techniques during a lower endoscopy procedure to stop the bleeding.
Doctors may recommend surgery to treat radiation proctopathy if other treatments don’t work or if you develop complications.
Diversion proctitis
If you develop diversion proctitis after ostomy surgery of the bowel, doctors may recommend surgery to close the ostomy and reconnect your rectum to the rest of your intestines. After surgery, waste will move through the intestines and pass through the rectum and anus again. Diversion proctitis typically goes away after surgery.
If you cannot have surgery to reconnect your rectum to the rest of your intestines, your doctor may recommend medicines to treat diversion proctitis, including medicines you insert into your rectum such as suppositories and enemas.
Proctitis due to other causes
Doctors may recommend treating the causes of other types of proctitis.
- If an injury to the anus or rectum causes proctitis, doctors may recommend avoiding the activity causing the injury.
- If taking nonsteroidal anti-inflammatory drugs (NSAIDs) causes proctitis, doctors may recommend stopping or changing your medicines.
- If lack of blood flow to the rectum causes proctitis, doctors may recommend treatments to increase blood flow.
Doctors may also recommend medicines to help reduce proctitis symptoms.
How do doctors treat the complications of proctitis?
Doctors may recommend surgery to treat complications of proctitis, such as abscesses, fistulas, or strictures. Doctors may also recommend surgery to treat proctitis if other treatments don’t work.
Can proctitis be prevented?
You can lower your risk for infectious proctitis by taking steps to prevent sexually transmitted infections and food poisoning. Doctors who treat cancer with radiation therapy have developed methods to lower the risk of radiation proctopathy.
However, experts haven’t found ways to prevent other types of proctitis.
Clinical Trials
The NIDDK conducts and supports clinical trials in many diseases and conditions, including digestive diseases. The trials look to find new ways to prevent, detect, or treat disease and improve quality of life.
What are clinical trials for proctitis?
Clinical trials—and other types of clinical studies—are part of medical research and involve people like you. When you volunteer to take part in a clinical study, you help doctors and researchers learn more about disease and improve health care for people in the future.
Researchers are studying many aspects of proctitis, such as new treatments for this condition.
Find out if clinical studies are right for you.
Watch a video of NIDDK Director Dr. Griffin P. Rodgers explaining the importance of participating in clinical trials.
What clinical studies for proctitis are looking for participants?
You can find clinical studies on proctitis at ClinicalTrials.gov. In addition to searching for federally funded studies, you can expand or narrow your search to include clinical studies from industry, universities, and individuals; however, the National Institutes of Health does not review these studies and cannot ensure they are safe. Always talk with your health care provider before you participate in a clinical study.
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank:
Brooks D. Cash, M.D., University of Texas McGovern Medical School

