Glomerular Disease Primer: Kidney Disease
- End-Stage Kidney Disease
- Glomerular Disease Syndromes
- Remission of Glomerular Disease
- Classification of Glomerular Diseases
- Assessing Progressive Loss of Glomerular Filtration Rate (GFR)
- Stages of Chronic Kidney Disease (CKD)
End-stage Kidney Disease
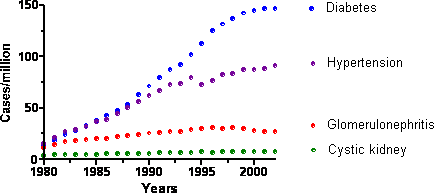
End-stage kidney disease (ESKD) is a major health problem in the US and other developed countries. ESKD occurs when patient survival requires a treatment, either chronic dialysis or kidney transplant. In the US, approximately 100,000 people reach ESKD each year and begin dialysis or undergo kidney transplant surgery. In the US, the major causes of ESKD are diabetes, hypertension, glomerulonephritis, and cystic kidney disease (primarily polycystic kidney disease). As shown in the figure below, the rates of ESKD due to diabetes and hypertension have increased sharply over the past 20 years, but the rate of increase appears to have slowed recently.
Glomerular Disease Syndromes
Traditionally glomerular diseases are divided into those that present with nephritic syndrome and those that present with nephrotic syndrome. These syndromes have different presentations, as listed below, but they have an important commonality: proteinuria (an increase in the amount of protein in the urine). Normally, in adults, the kidneys excrete up to 150 mg/d (0.15 g/d) of protein. Proteinuria is a common manifestation of kidney injury, including both tubular injury and glomerular injury. Glomerular diseases interfere with the normal function of the glomerular filtration barrier and can increase protein excretion above 2 g/d. Nephrotic-range proteinuria is defined as protein excretion >3.5 g/d in adults.
Nephritic Syndrome
- hypertension, microscopic hematuria (blood visible in urine under the microscope but not necessarily visible with the naked eye)
- red blood cell casts in the urine
- proteinuria (often <2 g/d in adults)
Nephrotic Syndrome
- proteinuria >3.5 g/d in adults and >40 mg/kg in children (this will appear as 3 on urine protein dipstick) edema, which is the accumulation of salt water that the kidneys have not excreted; the fluid initially accumulates in the legs (shown below, pitting edema – the skin has a sustained dimple when pressure is placed)
- low serum albumin, the major serum protein
- elevated serum cholesterol, which is produced by the liver in response to proteinuria

Remission of Glomerular Disease
Remission is defined as the complete or partial resolution of disease manifestations, with the precise definition specific to the particular disease. Relapse means the return of disease manifestations after a remission has occurred.
Remission in Nephrotic Disease
The following definitions are consensus definitions but are not universally accept.
| Complete Remission | Partial Remission | |
|---|---|---|
| Children |
Definition 1: Urine dipstick negative or trace Definition 2: First morning urine protein/creatinine ratio < |
First morning urine protein/creatinine ratio <2 |
| Adults | 24 hour urine protein <0.3 g/d |
Definition 1: 24 hour urine protein – 50% fall from baseline and <3.5 g/d Definition 2: 24 hour urine protein <2 g/d |
Classification of Glomerular Disease
Glomerular diseases can be classified by the injury mechanism or glomerular cell target, by the presence or absence of systemic disease, and by the appearance of nephritic syndrome or nephrotic syndrome.
| Injury | Systemic or primary | Nephritic syndrome | Nephritic syndrome or isolated proteinuria |
|---|---|---|---|
| Immunologic | Systemic disease |
|
Membranous nephropathy associated with hepatitis B or lupus |
| Immunologic | Primary kidney disease |
|
Membranous nephropathy |
| Genetic | Systemic disease |
|
Fabry disease |
| Metabolic | Systemic disease | -- |
|
| Podocyte injury | Primary kidney disease | -- |
|
Assessing Progressive Loss of Glomerular Filtration Rate (GFR)
Serum creatinine rises as GFR falls, since creatinine is normally excreted by glomerular filtration. The relationship between GFR and serum creatinine is not linear and so following the level of serum creatinine is not a precise way to determine how rapidly GFR is falling.
Creatinine clearance is an approximate measure of GFR and is calculated using a formula that includes serum creatinine, urine creatinine (typically from a 24 hour urine collection) and urine volume. This is a good way to estimate GFR in patients with normal kidney function. The results can be expressed as ml/min or as ml/min/1.73 m2 (adjusted to the patients’s body surface area).
Estimated GFR (eGFR) can be determined using a formula that includes age, race, sex and serum creatinine (the MDRD equation or Levy equation). eGFR is expressed as ml/min/1.73m2. Even when creatinine clearance is expressed as ml/min/1.73m2, it tends to be higher than eGFR.
Importantly, however GFR is measured, the kidney has enormous functional reserve. This allows a healthy individual to donate a kidney for the purposes of renal transplantation and the serum creatinine remains within the normal range. Thus a major limitation of serum creatinine (and all the above measurements) is that it remains within the normal range until extensive kidney damage has occurred.
Stages of Chronic Kidney Disease (CKD)
NKF: https://www.kidney.org/professionals/guidelines
| eGFR | Stage of Kidney Disease |
|---|---|
| >90 ml/min/1.73m2 | Normal kidney function (early kidney disease may or may not be present) |
| 60-90 ml/min/1.73m2 | Mild CKD |
| 30-59 ml/min/1.73m2 | Moderate CKD |
| 15-29 ml/min/1.73m2 | Severe CKD |
| <15 ml/min/1.73m2 | End-stage kidney disease |
