Renal Artery Stenosis
On this page:
- What are renal artery stenosis (RAS) and renovascular hypertension (RVH)?
- What are the kidneys and what do they do?
- What causes RAS?
- Who is at risk for RAS?
- What are the symptoms of RAS?
- What are the possible complications of RAS?
- How is RAS diagnosed?
- How is RAS treated?
- Eating, Diet, and Nutrition
- Clinical Trials
What are renal artery stenosis (RAS) and renovascular hypertension (RVH)?
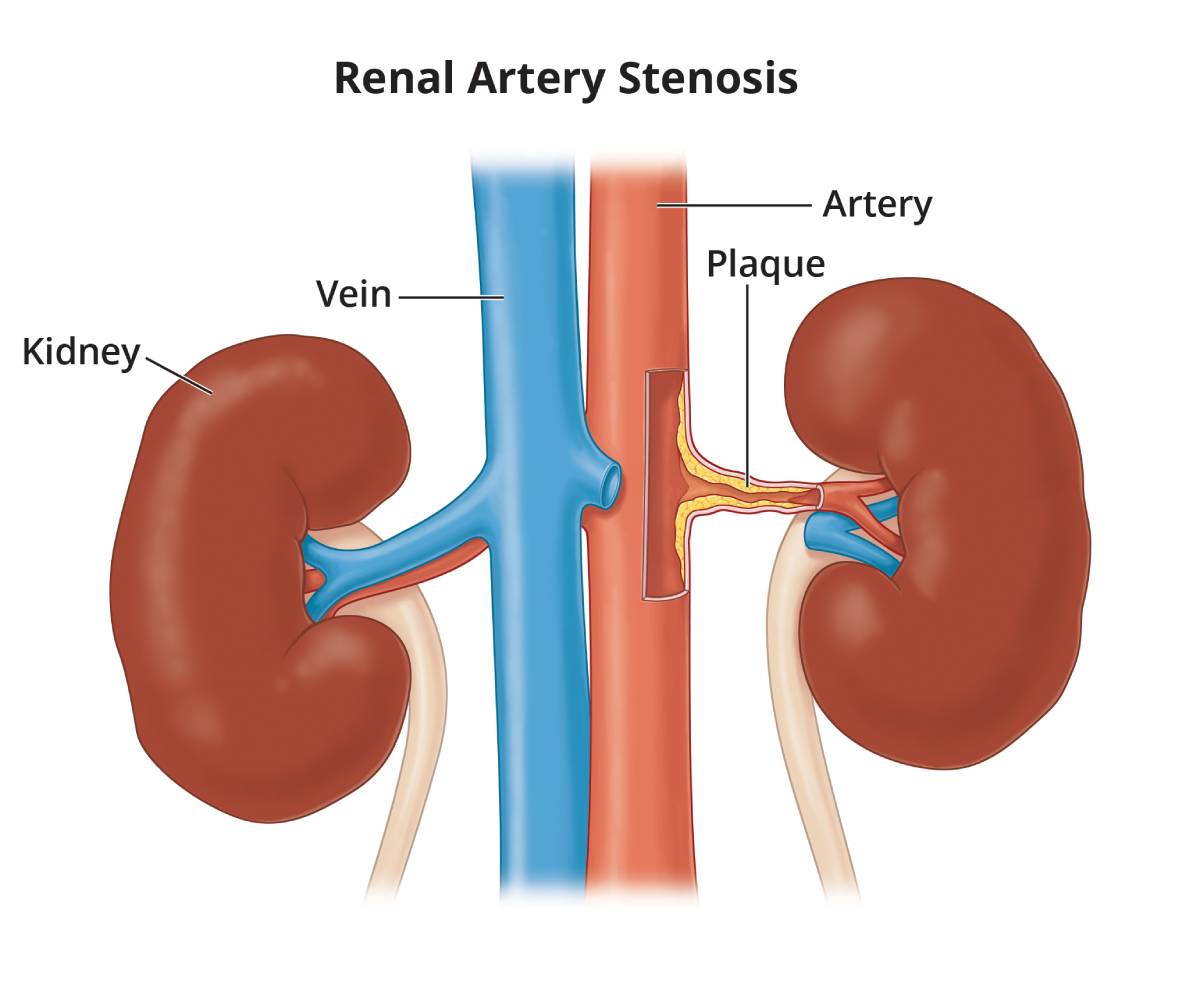
Renal artery stenosis (RAS) is the narrowing of one or both renal arteries. “Renal” means “kidney” and “stenosis” means “narrowing.” The renal arteries are blood vessels that carry blood to the kidneys from the aorta—the main blood vessel that carries blood from the heart to arteries throughout the body.
Renovascular hypertension (RVH) is high blood pressure caused by RAS. Blood pressure is written with two numbers separated by a slash, 120/80, and is said as “120 over 80.” The top number is called the systolic pressure and represents the pressure as the heart beats and pushes blood through the blood vessels. The bottom number is called the diastolic pressure and represents the pressure as blood vessels relax between heartbeats. A person’s blood pressure is considered normal if it stays at or below 120/80. High blood pressure is a systolic pressure of 140 or above or a diastolic pressure of 90 or above.1
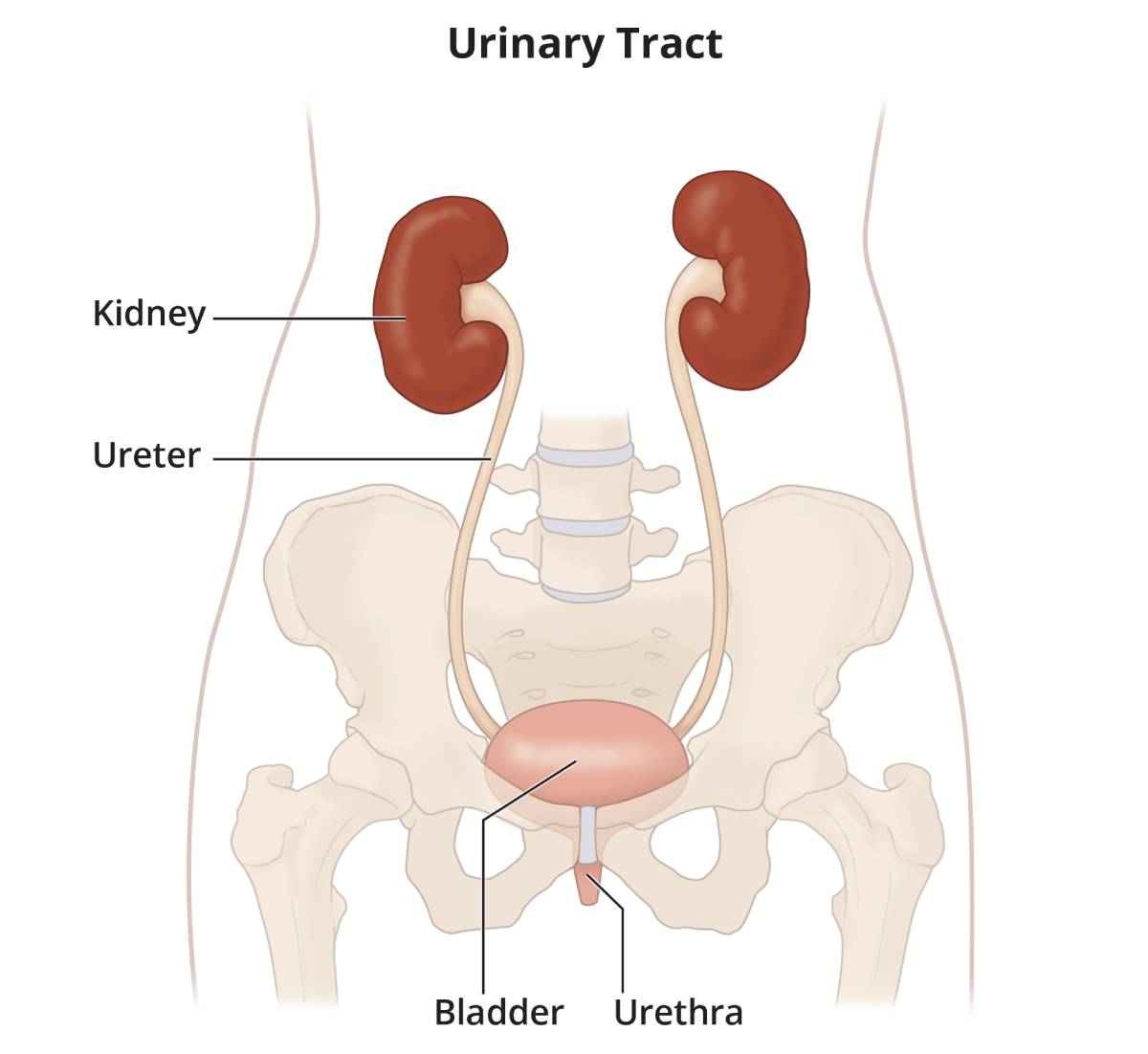
What are the kidneys and what do they do?
The kidneys are two bean-shaped organs, each about the size of a fist. They are located just below the rib cage, one on each side of the spine. Every day, the two kidneys filter about 120 to 150 quarts of blood to produce about 1 to 2 quarts of urine, composed of wastes and extra fluid.
 View full-sized image
View full-sized image What causes RAS?
About 90 percent of RAS is caused by atherosclerosis—clogging, narrowing, and hardening of the renal arteries.2 In these cases, RAS develops when plaque—a sticky substance made up of fat, cholesterol, calcium, and other material found in the blood—builds up on the inner wall of one or both renal arteries. Plaque buildup is what makes the artery wall hard and narrow.
Most other cases of RAS are caused by fibromuscular dysplasia (FMD)—the abnormal development or growth of cells on the renal artery walls—which can cause blood vessels to narrow. Rarely, RAS is caused by other conditions.
Who is at risk for RAS?
People at risk for artherosclerosis are also at risk for RAS. Risk factors for RAS caused by artherosclerosis include
- high blood cholesterol levels
- high blood pressure
- smoking
- insulin resistance
- diabetes
- being overweight or having obesity
- lack of physical activity
- a diet high in fat, cholesterol, sodium, and sugar
- being a man older than 45 or a woman older than 55
- a family history of early heart disease
The risk factors for RAS caused by FMD are unknown, but FMD is most common in women and people 25 to 50 years of age.3 FMD can affect more than one person in a family, indicating that it may be caused by an inherited gene.
What are the symptoms of RAS?
In many cases, RAS has no symptoms until it becomes severe.
The signs of RAS are usually either high blood pressure or decreased kidney function, or both, but RAS is often overlooked as a cause of high blood pressure. RAS should be considered as a cause of high blood pressure in people who
- are older than age 50 when they develop high blood pressure or have a marked increase in blood pressure
- have no family history of high blood pressure
- cannot be successfully treated with at least three or more different types of blood pressure medications
Symptoms of a significant decrease in kidney function include
- increase or decrease in urination
- edema—swelling, usually in the legs, feet, or ankles and less often in the hands or face
- drowsiness or tiredness
- generalized itching or numbness
- dry skin
- headaches
- weight loss
- appetite loss
- nausea
- vomiting
- sleep problems
- trouble concentrating
- darkened skin
- muscle cramps
What are the possible complications of RAS?
People with RAS are at increased risk for complications resulting from loss of kidney function or atherosclerosis occurring in other blood vessels, such as
- chronic kidney disease (CKD)—reduced kidney function over a period of time
- coronary artery disease—narrowing and hardening of arteries that supply blood to the heart
- stroke—brain damage caused by lack of blood flow to the brain
- peripheral vascular disease—blockage of blood vessels that restricts flow of blood from the heart to other parts of the body, particularly the legs
RAS can lead to kidney failure, described as end-stage renal disease when treated with blood-filtering treatments called dialysis or a kidney transplant, though this is uncommon in people who receive ongoing treatment for RAS.
How is RAS diagnosed?
A health care provider can diagnose RAS by listening to the abdomen with a stethoscope and performing imaging tests. When blood flows through a narrow artery, it sometimes makes a whooshing sound, called a bruit. The health care provider may place a stethoscope on the front or the side of the abdomen to listen for this sound. The absence of this sound, however, does not exclude the possibility of RAS.
In some cases, RAS is found when a person has a test for another reason. For example, a health care provider may find RAS during a coronary angiogram for diagnosis of heart problems. A coronary angiogram is a procedure that uses a special dye, called contrast medium, and x-rays to see how blood flows through the heart.
The following imaging tests are used to diagnose RAS:
- Duplex ultrasound. Duplex ultrasound combines traditional ultrasound with Doppler ultrasonography. Traditional ultrasound uses a device, called a transducer, that bounces safe, painless sound waves off organs to create an image of their structure. Doppler ultrasonography records sound waves reflected off of moving objects, such as blood, to measure their speed and other aspects of how they flow. The procedure is performed in a health care provider’s office, outpatient center, or hospital by a specially trained technician, and the images are interpreted by a radiologist—a doctor who specializes in medical imaging. Anesthesia is not needed. The images can show blockage in the renal artery or blood moving through nearby arteries at a lower-than-normal speed. Ultrasound is noninvasive and low cost.
- Catheter angiogram. A catheter angiogram, also called a traditional angiogram, is a special kind of x-ray in which a thin, flexible tube called a catheter is threaded through the large arteries, often from the groin, to the artery of interest—in this case, the renal artery. The procedure is performed in a hospital or outpatient center by a radiologist. Anesthesia is not needed though a sedative may be given to lessen anxiety during the procedure. Contrast medium is injected through the catheter so the renal artery shows up more clearly on the x-ray. Catheter angiogram is the “gold standard” for diagnosing RAS due to the high quality of the image produced. In addition, severe RAS can be treated during the same visit. However, a catheter angiogram is an invasive procedure, and a person may have side effects from the sedative or contrast medium or may have bleeding or injury to the artery from the catheter. The procedure is also more expensive than other imaging tests.
- Computerized tomographic angiography (CTA) scan. CTA scans use a combination of x-rays and computer technology to create images. The procedure is performed in an outpatient center or hospital by an x-ray technician, and the images are interpreted by a radiologist. Anesthesia is not needed. Contrast medium is injected into a vein in the person’s arm to better see the structure of the arteries. CTA scans require the person to lie on a table that slides into a tunnel-shaped device where the x-rays are taken. CTA scans are less invasive than catheter angiograms and take less time. However, the risks from the x-ray radiation still exist, and the test often requires more contrast medium than a catheter angiogram, so it may not be recommended for a person with poor kidney function.
- Magnetic resonance angiogram (MRA). MRA uses radio waves and magnets to produce detailed pictures of the body’s internal organs and soft tissues without using x-rays. The procedure is performed in an outpatient center or hospital by an x-ray technician, and the images are interpreted by a radiologist. Anesthesia is not needed though light sedation may be used for people with a fear of confined spaces. Contrast medium may be injected into a vein in the person’s arm to better see the structure of the arteries. With most MRA scans, the person lies on a table that slides into a tunnel-shaped device that may be open ended or closed at one end; some newer machines are designed to allow the person to lie in a more open space. In addition to providing high-quality images noninvasively, MRA can provide a functional assessment of blood flow and organ function. However, the use of contrast medium for an MRA is not advised for people with poor kidney function because of the risk of complications to the skin and other organs if the kidneys do not remove the contrast medium well enough.
How is RAS treated?
Treatment for RAS includes lifestyle changes, medications, and surgery and aims to
- prevent RAS from getting worse
- treat RVH
- relieve the blockage of the renal arteries
RAS that has not led to RVH or caused a significant blockage of the artery may not need treatment. RAS that needs to be treated, also called critical RAS, is defined by the American Heart Association as a reduction by more than 60 percent in the diameter of the renal artery.1 However, health care providers are not exactly sure what degree of blockage will cause significant problems.
Lifestyle Changes
The first step in treating RAS is making lifestyle changes that promote healthy blood vessels throughout the body, including the renal arteries. The best ways to keep plaque from building up in the arteries are to exercise, maintain a healthy body weight, and choose healthy foods. People who smoke should quit to help protect their kidneys and other internal organs.
Medications
People with RVH may need to take medications that—when taken as prescribed by their health care provider—lower blood pressure and can also significantly slow the progression of kidney disease. Two types of blood pressure-lowering medications, angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), have proven effective in slowing the progression of kidney disease. Many people require two or more medications to control their blood pressure. In addition to an ACE inhibitor or an ARB, a diuretic—a medication that helps the kidneys remove fluid from the blood—may be prescribed. Beta blockers, calcium channel blockers, and other blood pressure medications may also be needed. Some people with RAS cannot take an ACE inhibitor or ARB due to the effects on the kidneys. People with RAS who are prescribed an ACE inhibitor or ARB should have their kidney function checked within a few weeks of starting the medication.
A cholesterol-lowering medication to prevent plaque from building up in the arteries and a blood-thinner, such as aspirin, to help the blood flow more easily through the arteries may also be prescribed.
Surgery
Although surgery has been used in the past for treatment of RAS due to atherosclerosis, recent studies have not shown improved outcomes with surgery compared with medication. However, surgery may be recommended for people with RAS caused by FMD or RAS that does not improve with medication. Different types of surgery for RAS include the following. The procedures are performed in a hospital by a vascular surgeon—a doctor who specializes in repairing blood vessels. Anesthesia is needed.
- Angioplasty and stenting. Angioplasty is a procedure in which a catheter is put into the renal artery, usually through the groin, just as in a catheter angiogram. In addition, for angioplasty, a tiny balloon at the end of the catheter can be inflated to flatten the plaque against the artery wall. A small mesh tube, called a stent, may then be positioned inside the artery to keep plaque flattened and the artery open. People with RAS caused by FMD may be successfully treated with angioplasty alone, while angioplasty with stenting has a better outcome for people with RAS caused by atherosclerosis.
- Endarterectomy or bypass surgery. In an endarterectomy, the plaque is cleaned out of the artery, leaving the inside lining smooth and clear. To create a bypass, a vein or synthetic tube is used to connect the kidney to the aorta. This new path serves as an alternate route for blood to flow around the blocked artery into the kidney. These procedures are not performed as often as in the past due to a high risk of complications during and after the procedure.
Eating, Diet, and Nutrition
Limiting intake of fats, cholesterol, sodium, and sugar can help prevent atherosclerosis, which can lead to RAS. Most sodium in the diet comes from salt. A healthy diet that prevents people from becoming overweight or developing obesity can also help prevent atherosclerosis. People with RAS that has caused decreased kidney function should limit their intake of protein, cholesterol, sodium, and potassium to slow the progression of kidney failure. More information about nutrition for CKD is provided in the NIDDK health topics, Eating Right for Chronic Kidney Disease and Diet & Nutrition for Adults with Advanced Chronic Kidney Disease. People should talk with their health care provider about what diet is right for them.
Clinical Trials
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into many diseases and conditions.
What are clinical trials, and are they right for you?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you.
What clinical trials are open?
Clinical trials that are currently open and are recruiting can be viewed at ClinicalTrials.gov.
References
This content is provided as a service of the National Institute of Diabetes and Digestive and Kidney Diseases
(NIDDK), part of the National Institutes of Health. NIDDK translates and disseminates research findings to increase knowledge and understanding about health and disease among patients, health professionals, and the public. Content produced by NIDDK is carefully reviewed by NIDDK scientists and other experts.
The NIDDK would like to thank:
Christopher Cooper, M.D., University of Toledo

